 A recent study developed at the University of Illinois at Chicago (UIC) revealed a novel molecular mechanism that sustains the integrity of cells lining the lung’s blood vessels, forming a leak-proof barrier. The study led by Asrar Malik and entitled “HIF2α signaling inhibits adherens junctional disruption in acute lung injury” was published in the Journal of Clinical Investigation.
A recent study developed at the University of Illinois at Chicago (UIC) revealed a novel molecular mechanism that sustains the integrity of cells lining the lung’s blood vessels, forming a leak-proof barrier. The study led by Asrar Malik and entitled “HIF2α signaling inhibits adherens junctional disruption in acute lung injury” was published in the Journal of Clinical Investigation.
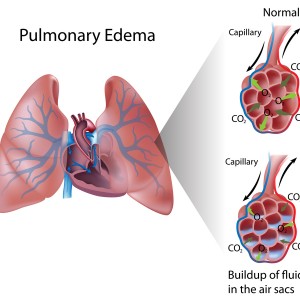
Dysfunction of the vascular endothelial barrier can trigger acute respiratory distress syndrome (ARDS). ARDS is a severe, often fatal condition, characterized by inflammation and fluid accumulation (edema) in lungs due to leaky blood vessels. Few therapies can be successfully applied to reverse this fluid leakage, with supportive care being the current standard treatment, namely by artificial ventilation.
In a normal immune response to infection, the endothelial barrier in the blood vessels loosens temporarily, so that white blood cells can exit the bloodstream and fight the bacteria or virus foreigner to the body. However, in certain situations, this barrier is not properly restored resulting in leakiness of blood vessels. This is particularly troublesome in the lung. By a natural mechanism, as fluid leaks into the lungs and the blood becomes under-oxygenated, the cells lining the blood vessels get tighter; unfortunately, this tightening of the barrier in response to low oxygen is not fast enough in ARDS patients.
“It’s a vicious cycle of inflammation and leakiness of the lung blood vessels that is very hard to control,” said Dr. Jalees Rehman, one of the lead authors of the study. “It’s as if the lung is drowning in its body’s own fluids. Being able to prevent this by stabilizing and restoring the integrity of the blood vessel barrier could help save lives.”
[adrotate group=”3″]
The researchers analyzed several proteins that regulate cell-to-cell contacts, also known as adherens junctions, and found that the VE-PTP protein can increase the integrity of the endothelial barrier. This VE-PTP is regulated by a factor sensitive to oxygen levels – HIF2α. Low-oxygen conditions induce expression of HIF2α and subsequently VE-PTP. Mice lacking the HIF2α factor had a decreased expression of VE-PTP resulting in defective adherens junctions and increased lung vascular permeability. Interestingly, the team found that if they treated mice that had been exposed to bloodstream infections with a specific molecule – Fg4497 – the expression of HIF2α /VE-PTP was activated resulting in an induction of a cell-tightening mechanism, thus preventing the loss of endothelial barrier integrity and leakiness of blood vessels. These mice had higher survival rates and less fluid in their lungs compared to mice that did not receive the treatment.
“Our current studies were conducted in mice, but we hope that one day we will be able to take advantage of the body’s natural response to low blood oxygen levels with drugs that mimics low oxygen conditions. These drugs could be given to high-risk patients and hopefully prevent the formation of ARDS by activating the internal protective barrier tightening mechanism,” stated Rehman. The reported mechanism in this study therefore represents a potential new target for the treatment of inflammatory diseases, such as the life-threatening ARDS, by preventing the formation of leaky vessels and edema.

