A recently accepted manuscript on the Canadian Journal of Cardiology, an open access journal, provides an overview of the current clinical use of noninvasive imagining techniques, such as echocardiography, for pulmonary arterial hypertension (PAH). The study investigators, led by Dr. Irene Lang, MD, Professorship of Vascular Biology, Department of Internal Medicine, Division of Cardiology, Medical University of Vienna Austria, conducted a thoroughly researched review that highlights the present role non-invasive imaging has and its potential to eventually replace hemodynamics as the standard approach to screening, diagnosing and managing PAH.
PAH, also known as pulmonary arterial hypertension, causes breathlessness, loss of exercise capacity, and death due to elevated pulmonary artery pressure and subsequent right heart failure. It is a rare condition affecting 1 to 2 individuals for every 1 million in the US and Europe.
PAH is characterized by high blood pressure (BP) in the pulmonary arteries, which carry oxygen and blood from the heart to the lungs. This elevated arterial pressure causes the right ventricle of the heart, which supplies blood to the pulmonary arteries, to pump ineffectively. This results in the right side of the heart working harder to pump blood around the body, leading to the condition’s debilitating effects and the eventual pre-mature death of the patient.
PAH is most often inadvertently discovered after a patient undergoes a non-invasive echocardiography or an invasive right heart catheterization for another condition; as a result, it is generally not diagnosed until the disease is advanced and the right side of the heart begins to fail.
In an effort to better diagnose PAH when it is just presenting or in its earliest stages, pulmonary specialists who treat PAH are in need of new clinical guidelines that use an integrated approach that utilizes both invasive and non-invasive tools. To better understand where non-invasive imaging fits in this approach it is important to understand how it is currently used and what its potential uses could be in helping to lower the morbidity and mortality rates associated with PAH.
[adrotate group=”4″]
After thoroughly researching the use of non-invasive techniques to assess, diagnose, and manage PAH the study findings included:
- Transthoracic Doppler echocardiography is currently the most predominant method used to reliably assess PAH in the early stages of diagnosis.
- Significant progress has been made in the use of 2D imaging to create a 3D echo imaging computer model of the structure and function of the right ventricle.
- The 3D echo images have comparable measurement results to magnetic resonance imaging (MRI).
- In clinical practice, MRI of the pulmonary vessel system is still considered inferior to computed tomography (CT).
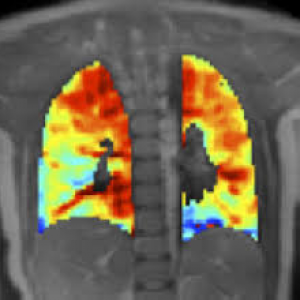
- There have been numerous important clinical advancements in non-invasive imaging modalities such as dual-energy CT, cone-beam CT, ECG gated 320-row Area Detector Computed. Tomography (ADCT), and lung perfusion MRI that are changing the clinical guidelines for diagnosing and treating PAH.
A non-invasive approach has numerous benefits to patients, such as a lowered risk of infection, reduced rehabilitation time, and reduced time lost from work. In light of the benefits, the results of this study are of great importance to patients and their healthcare providers for it assessed the usefulness and accuracy of taking a non-invasive approach to PAH management and treatment.

