 A team led by researchers at Georgia State University in Atlanta recently revealed a previously unknown mechanism behind the development of tolerance to the drug roflumilast used in the treatment of chronic obstructive pulmonary disease (COPD). The study was published in the journal Proceedings of the National Academy of Sciences and is entitled “Cross-talk between PKA-Cβ and p65 mediates synergistic induction of PDE4B by roflumilast and NTHi.”
A team led by researchers at Georgia State University in Atlanta recently revealed a previously unknown mechanism behind the development of tolerance to the drug roflumilast used in the treatment of chronic obstructive pulmonary disease (COPD). The study was published in the journal Proceedings of the National Academy of Sciences and is entitled “Cross-talk between PKA-Cβ and p65 mediates synergistic induction of PDE4B by roflumilast and NTHi.”
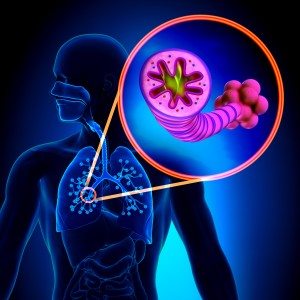
COPD is a progressive disease in which individuals develop serious breathing-related problems such as obstruction of the airways, wheezing, shortness of breath (dyspnea), chest tightness and acute exacerbations. It is one of the most common lung diseases and the fourth-leading cause of death worldwide. Cigarette smoking is considered to be the leading cause of COPD. Exacerbations and co-morbidities contribute to disease severity.
In 2011, the U.S. Food and Drug Administration (FDA) approved a new drug, roflumilast (commercially known as Daliresp) for COPD treatment, namely to reduce the frequency of flare-ups or worsening of the disease symptoms. However, it has been reported that patients can develop tolerance for the drug.
Researchers now found that roflumilast induces the production of a protein that leads to inflammation, which may facilitate the development of drug tolerance by patients after repeated uses, making roflumilast treatment less effective. “There is clinical evidence showing that patients could develop a tolerance if they keep taking repeated dosing of this drug, but why or how has been unknown. If we can figure out why people have a tolerance, we can probably improve the therapeutics,” said the study’s senior author Dr. Jian-Dong Li in a news release.
[adrotate group=”3″]
Roflumilast works by inhibiting the activity of an enzyme called phosphodiesterase 4B (PDE4B), which ultimately leads to a decrease in inflammation and relaxation of the airway’s smooth muscle, easing COPD symptoms. Researchers now found that roflumilast also triggers an undesired process in combination with nontypeable Haemophilus influenzae (the major bacterial pathogen that causes COPD exacerbations) leading to an increase in the production of PDE4B2 and consequently an increase in inflammation (via both enzymatic activity-dependent and activity-independent manners) that may contribute to the development of tolerance to roflumilast. Researchers also found that the protein kinase A catalytic subunit β (PKA-Cβ) and nuclear factor-κB (NF-κB) p65 subunit are required for the induction of PDE4B2 production.
“We found there is some inflammatory response which cannot be suppressed by the drug because it has little to do with the enzyme activity,” explained Dr. Li. “The patient keeps taking the drug and over time, you give more drug and you produce more target protein, which is even more counterproductive for suppressing inflammation. Over time, we develop a tolerance.”
The research team concluded that this previously unknown mechanism underlying the up-regulation of PDE4B2 protein may explain the development of tolerance to roflumilast treatment, and may help in the development of new therapeutic strategies to improve the efficacy of roflumilast.

