There is a thick accumulation of mucus in cystic fibrosis patients’ lungs that clogs the airways over time. This phenomenon leads to a growing cluster of bacteria in the pulmonary region, which often times triggers recurrent infections.
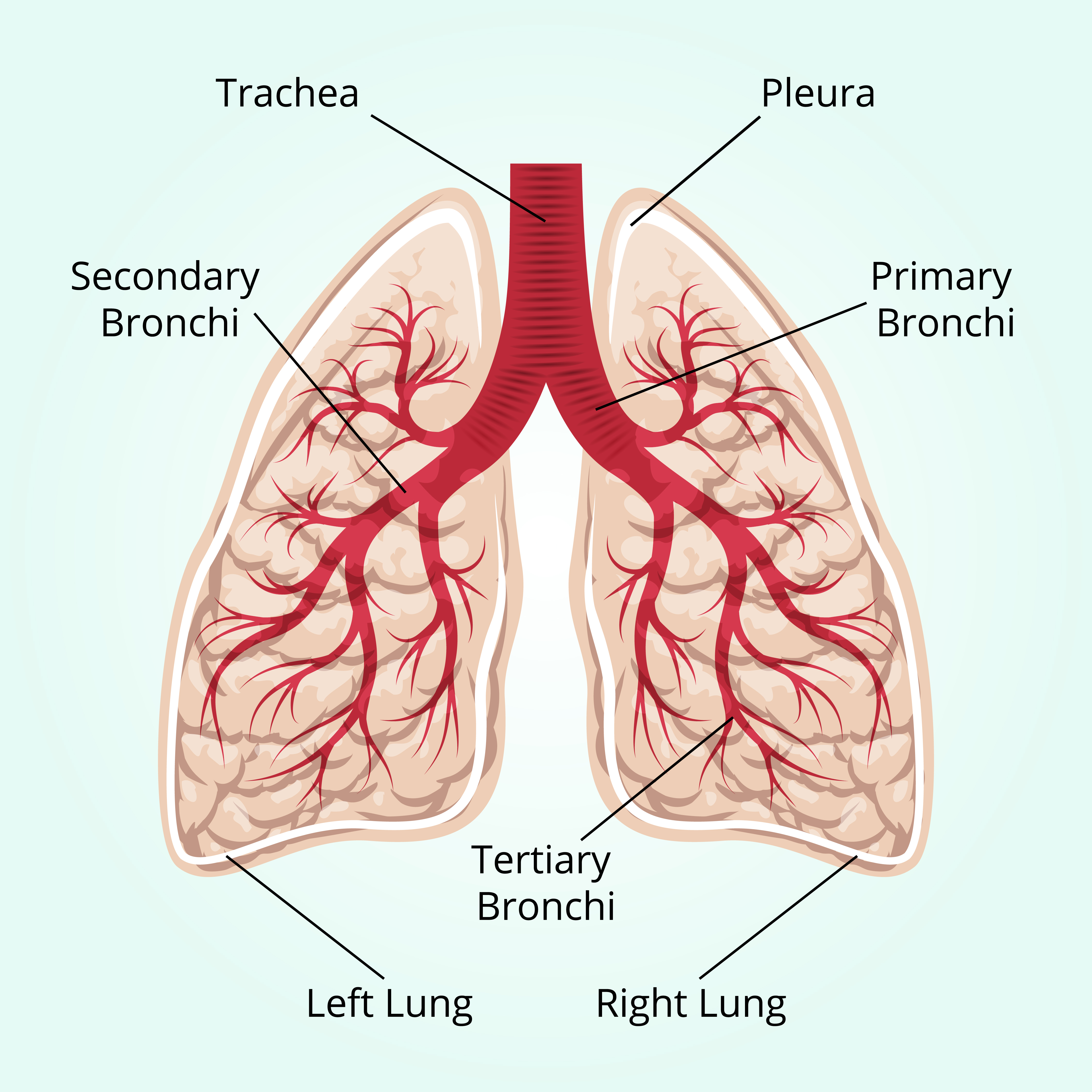
A recent study published in the Cell Host & Microbe entitled “Regional Isolation Drives Bacterial Diversification within Cystic Fibrosis Lungs” demonstrates that the same treatments used for CF patients can feature different levels of efficacy in treating bacterial infections depending on the region of the lung where bacteria settle. A collection of bacteria might begin with one bacterial lineage, but over time these clusters evolve, becoming isolated from each other and developing region-specific traits. These differences have been implicated in the increasing issue of antibiotic resistance.
In order to understand how this resistance to antibiotics and immune defense works in clusters of bacteria, a research group at the Washington School of Medicine collected samples of bacteria from different regions of cystic fibrosis lungs. The study revealed that even though there were different bacterial populations in various regions, all of them descended from the same bacterial strain. This finding suggests that in each lung region there were diverse bacteria with distinct properties. According to Dr. Peter Jorth, member of the research group, the relevance of this observation is that it showed that in each lung region, bacterial resistance to antibiotics and virulence varied and consequently this variation might affect patients’ health ad treatment options.
Moreover, after comparing the bacterial genetic code, it was clear that bacteria had differentiated locally after exposure to different environments in each region of the lung. Another model even followed Darwin’s evolution model.
It was also observed through DNA analysis that even though bacteria inhabiting different lung regions do not show evidence of one specific trait, they may have “genetic memory,” which allows them to trigger specific responses when coming in contact with particular environmental conditions. In order words, bacteria can strengthen their resistance to treatments by activating certain codes in their genetic memory.
The author of the study, Dr. Pradeep Singh, noted that “even when a single strain of bacteria causes a chronic infection, evolution with human organs can produce diverse families of related bacteria”. This is why after a treatment starts weakening one bacterial population, another bacterial sibling can begin to grow that is functionally stronger and resistant. It is their genetic code and memory that are able to allow them to react to the treatment and resist it.
The next step of the research will be to understand how bacteria develop this memory and design mechanisms to attack diverse bacterial populations in order to improve treatment efficiency.