 Quick: what’s the third leading cause of death in the U.S.? I doubt that many would have answered: “Chronic Obstructive Pulmonary Disease,” but according to the Centers for Disease Control and Prevention, COPD ranks third (138,080) after Heart disease (597,689) and cancers (574,743). The American Lung Association notes that COPD is also a major cause of disability, and while some 12 millions Americans have a formal COPD diagnosis. An estimated 12 million more people may have the disease and go undiagnosed. Approximately 23 million men and women in the United States have COPD.
Quick: what’s the third leading cause of death in the U.S.? I doubt that many would have answered: “Chronic Obstructive Pulmonary Disease,” but according to the Centers for Disease Control and Prevention, COPD ranks third (138,080) after Heart disease (597,689) and cancers (574,743). The American Lung Association notes that COPD is also a major cause of disability, and while some 12 millions Americans have a formal COPD diagnosis. An estimated 12 million more people may have the disease and go undiagnosed. Approximately 23 million men and women in the United States have COPD.
COPD is a term that like “cancer,” actually encompasses a range of conditions, but generally speaking refers to permanent lung damage that gets worse over time. The disease can affect patients’ airways, air sacs or both The disease can affect patients’ lung airways, air sacs or both. The two most prevalent forms of COPD are chronic bronchitis and emphysema. Both cause airway blockage, resulting in shortness of breath, chronic productive coughing that produces large amounts of mucus, chest tightness and/or wheezing and other symptoms. Laboring to breathe can limit activity, diminish quality of life and put extra strain on the heart.
The leading cause of COPD is cigarette smoking. According to the National Institutes of Health, 42 percent of COPD sufferers are former smokers and 34 percent are current smokers. However, the rest — a substantial 24 percent — are people who’ve never lit a cigarette, and it is believed that exposure to other lung irritants such as air pollution, chemical fumes, or dust, especially over long terms, also may contribute to development of COPD.
In terms of the two principal COPD categories, in emphysema, the walls between many of the lungs’ air sacs are damaged, losing their shape and becoming “floppy.” This damage also can destroy the walls of the air sacs, leading to fewer and larger air sacs instead of many tiny ones, and if this happens, the amount of gas exchange in the lungs is reduced.
In chronic bronchitis, the lining of the airways is constantly irritated and inflamed, causing it to thicken. Lots of thick mucus then forms in the airways, making it hard to breathe. Since most people who have COPD have both emphysema and chronic bronchitis the general term “COPD” is more comprehensively accurate.
In COPD, less air flows in and out of the airways because of one or more of the following:
• The airways and air sacs lose their elastic quality.
• The walls between many of the air sacs are destroyed.
• The walls of the airways become thick and inflamed.
• The airways make more mucus than usual, which can clog them.
In most instances COPD develops slowly, and symptoms often worsen over time limiting ability to do routine activities. Severe COPD may inhibit the patient from doing even basic activities like walking, cooking, or taking care of themselves. COPD is typically diagnosed in middle-aged or older adults, and is not contagious or communicable.
 There is also no cure for COPD as yet, with no known means of reversing damage to the airways and lungs, but some treatments and lifestyle changes can help patients feel better, stay more active, and slow the progress of the disease. Pulmonologist Kathrin Nicolacakis, MD, of the Cleveland Clinic in Cleveland Ohio affirms that “There is a lot that can be done for COPD patients. “People need to know that COPD is treatable, and if you have symptoms, there are many options to help you feel better. We may not be able to reverse it, but we can control the symptoms and prevent further damage to the lungs.”
There is also no cure for COPD as yet, with no known means of reversing damage to the airways and lungs, but some treatments and lifestyle changes can help patients feel better, stay more active, and slow the progress of the disease. Pulmonologist Kathrin Nicolacakis, MD, of the Cleveland Clinic in Cleveland Ohio affirms that “There is a lot that can be done for COPD patients. “People need to know that COPD is treatable, and if you have symptoms, there are many options to help you feel better. We may not be able to reverse it, but we can control the symptoms and prevent further damage to the lungs.”
According to the Cleveland Clinic, clinical treatment of COPD may involve drugs, such as steroids or inhaled medications called bronchodilators (“puffers”) that open airways or reduce airway inflammation, supplemental oxygen, and alpha-1-antitrypsin (A1AT) infusions if you have an inherited deficiency. PDE4 enzyme inhibitors can reduce inflammation in some patients. Flu and pneumonia vaccines and Pneumococcal vaccine every five years can help prevent pneumonia, but medications may lose effectiveness over time.
A procedure called lung volume reduction surgery also is available. The surgery usually is a last resort reserved for people with severe symptoms that have not improved with medication, and in the procedure surgeons remove damaged tissue from the lungs. In carefully selected patients, lung volume reduction surgery can improve shortness of breath, quality of life and survival, but there are downsides. The surgery has risks, including a prolonged recovery time and discomfort from the surgical scar, says pulmonologist Joseph Cicenia, MD.
Dr. Nicolacakis asks all of her COPD patients to quit smoking, eat a healthy diet, get plenty of exercise and keep up on their influenza and pneumonia vaccines. “Taking care of themselves in these ways can sometimes help offset the complications of COPD,” she observes.
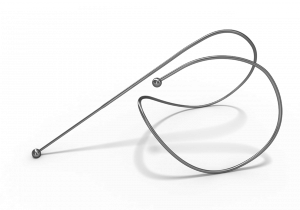
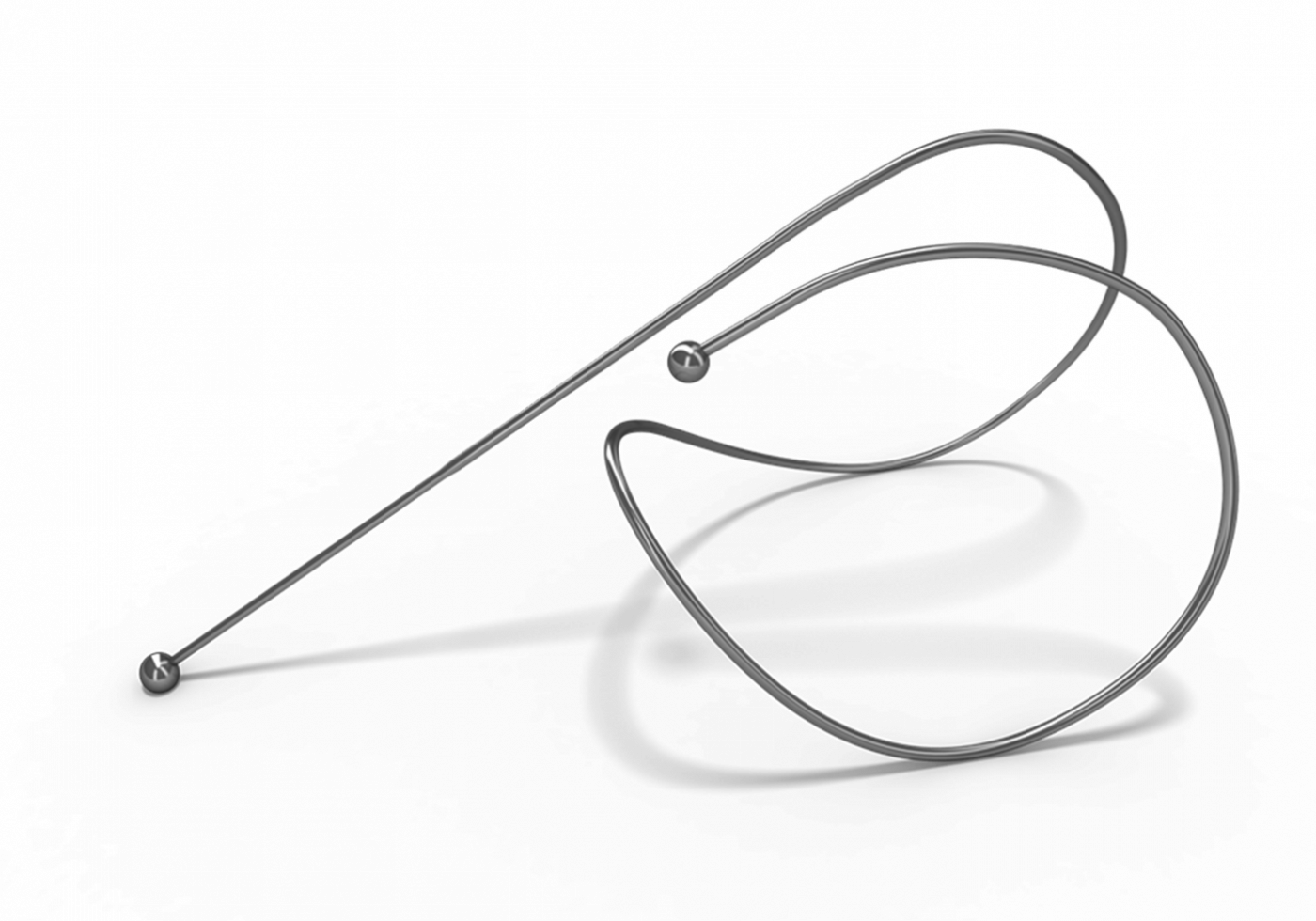
Currently, doctors and researchers are testing a new procedure to help COPD patients that doesn’t involve surgery that helps damaged lung tissue to regain elasticity lost to disease in clinical trials at Cleveland Clinic and other hospitals across the U.S. Doctors insert special flexible scopes through the patient’s mouth to place metal coils into the damaged tissue of the patient’s lung. The coils return elasticity to the diseased tissue, allowing the lungs to work in a more normal way.
 “We’re actually treating the lung by adding back elasticity to it that it had lost,” says Dr. Cicenia, who is one of the researchers in the clinical trial and has performed the procedure, in a Cleveland Clinic release. “When you lose elasticity it takes a lot longer to empty the lungs, which leads to the lungs hyperinflating. We’re actually treating the lung by adding back elasticity to it that it had lost. When you lose elasticity it takes a lot longer to empty the lungs, which leads to the lungs hyperinflating.”
“We’re actually treating the lung by adding back elasticity to it that it had lost,” says Dr. Cicenia, who is one of the researchers in the clinical trial and has performed the procedure, in a Cleveland Clinic release. “When you lose elasticity it takes a lot longer to empty the lungs, which leads to the lungs hyperinflating. We’re actually treating the lung by adding back elasticity to it that it had lost. When you lose elasticity it takes a lot longer to empty the lungs, which leads to the lungs hyperinflating.”
This hyperinflation, Dr. Cicenia says, is the key factor to why patients with COPD feel short of breath, noting that “If you add back lost elasticity, you reduce hyperinflation and potentially improve shortness of breath” he says.
The metal coils have been in use in Europe since 2008, and patients who received the coils as part of clinical studies there have reported substantial improvements in their lung function, capacity for exercise and quality of life. In general, the Cleveland Clinic researchers say patients recover from the coil procedure much more quickly than traditional surgery because it is non-invasive. Traditional surgery requires a large incision, or several small ones, in the chest to remove the diseased tissue. With the lung coil procedure, most patients go home after an overnight stay at the hospital.
“The preliminary results are promising,” says Dr. Cicenia. “Patients are having significant improvements in how far they can walk and their quality of life,” adding that preliminary studies have shown the coil procedure yields results that are comparable to the volume reduction surgery, but much safer and less invasive. “These early findings need to be confirmed in a larger clinical trial like the one we’re participating in now,” he observes.
The first signs of COPD may include a hacking cough with phlegm, shortness of breath, wheezing when you breathe or tightness in your chest For anyone finding that shortness of breath makes it too difficult to be physically active, Dr. Nicolacakis recommends seeing your doctor for a spirometry test, a simple outpatient procedure that assesses your lung function by measuring how much air you’re able to breathe in and out. If COPD is diagnosed Dr. Nicolacakis recommends pulmonary rehabilitation, where specialized respiratory therapists teach breathing techniques, exercises and proper nutrition to make living with COPD easier.
Sources:
Cleveland Clinic
Centers for Disease Control and Prevention
American Lung Association
National Institutes of Health
Image credits:
Cleveland Clinic
More resources and references:
http://health.clevelandclinic.org/2013/11/copd-4-myths-debunked/

At what stage can the tiny coils be inserted? I am at stage two and would like to do all i can to help it from progressing. I lost both my parents to COPD.
Thanks for all you are doing.