 Scientists from The Cancer Genome Atlas (TCGA) Research Network have identified novel mutations in a known cancer-causing signaling pathway leading to lung adenocarcinoma, one of the most frequent forms of lung-cancer.
Scientists from The Cancer Genome Atlas (TCGA) Research Network have identified novel mutations in a known cancer-causing signaling pathway leading to lung adenocarcinoma, one of the most frequent forms of lung-cancer.
Lung cancer is the most common cause of cancer-related death worldwide, causing more than 1 million deaths every year. Lung adenocarcinoma accounts for 40% of all lung cancers and develops in tissues near the outer parts of the lungs with the capacity to spread widely. Although smoking is the main risk factor, adenocarcinoma is still the most common type of lung cancer in lifelong non-smokers, with a 20 to 30% increased risk by exposure to secondhand smoke.
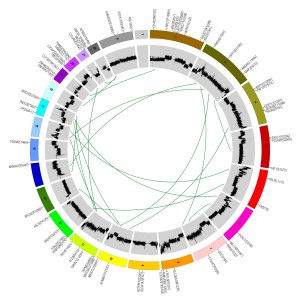
In this study, published in the journal Nature, the genomes, proteomes and RNAs from 230 lung adenocarcinoma samples were analyzed, resulting in the identification of specific mutations affecting the RTK/RAS/RAF pathway activity in 62% of the samples, causing it to become permanently activated and leading to cancer cell proliferation and survival.
The genes affected by these mutations are designated as oncogenes, since they have the potential to cause cancer when mutated or overly expressed. Mutations of several oncogenes integrating the RTK/RAS/RAF pathway were detected, such as amplification of ERBB2 and MET and mutations in NF1, a known tumor suppressor gene. Additionally, mutations in RIT1, a gene involved in regulating signaling cascades related to cellular stress, were also associated for the first time with lung cancer development.
“It is quite striking that we have now identified an actionable mutation in over 75 percent of patients with lung adenocarcinoma, a significant improvement from a decade ago,” said Matthew Meyerson, M.D., Ph.D., Harvard Medical School, Dana-Farber Cancer Institute, The Broad Institute, and one of the lead scientists on the project.
In 2012, TCGA reported the analysis of another, less common, form of lung cancer, squamous cell carcinoma, where a large number and variety of DNA alterations, many of which driving forces behind pathways that are important to the initiation and progression of lung cancer were found, becoming potential therapeutic targets.
“Combined with the earlier TCGA analysis of squamous lung cancers, we now have a comprehensive understanding of many of the genetic pathways that lead to cancers of the lung,” said NCI Director Harold Varmus, M.D. “Based on this knowledge, we can now seek better pathway inhibitors to improve patient outcomes. However, for the time being, stopping smoking or never starting remains the most reliable ways to reduce the number of deaths due to lung cancer.”
The discovery of these genomic changes can greatly increase the possible therapeutic targets for this disease, potentially identifying a bigger number of patients with treatable mutations, since many drugs already exist to correct the abnormal activity of this pathway.
“The integrated nature of TCGA analysis made these findings and their potential therapeutic implications possible,” said NIH Director Francis S. Collins, M.D., Ph.D. “We hope this lays the groundwork for future work in precision medicine.”
TCGA consists of more than 150 scientists at different institutions across the country and is jointly funded and managed by the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI), both part of the National Institutes of Health.

