 Researchers are offering new insights into the effects that cardiac arrhythmias have on mortality risk in Pulmonary Arterial Hypertension patients. A new study, entitled “Frequency of Supraventricular Arrhythmias in Patients With Idiopathic Pulmonary Arterial Hypertension,” was published in the American Journal of Cardiology led by first author Dr. Li Wen from the Department of Cardio-Pulmonary Circulation, Tongji University School of Medicine, Shanghai, China and Dr. Zhi-Cheng Jing, senior author of the study, from the Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, China. The study could help lead to new PAH treatment best practices.
Researchers are offering new insights into the effects that cardiac arrhythmias have on mortality risk in Pulmonary Arterial Hypertension patients. A new study, entitled “Frequency of Supraventricular Arrhythmias in Patients With Idiopathic Pulmonary Arterial Hypertension,” was published in the American Journal of Cardiology led by first author Dr. Li Wen from the Department of Cardio-Pulmonary Circulation, Tongji University School of Medicine, Shanghai, China and Dr. Zhi-Cheng Jing, senior author of the study, from the Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, China. The study could help lead to new PAH treatment best practices.
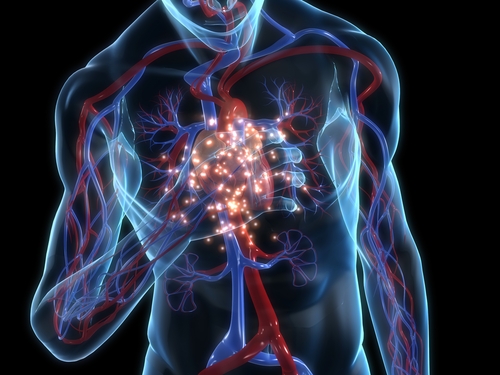
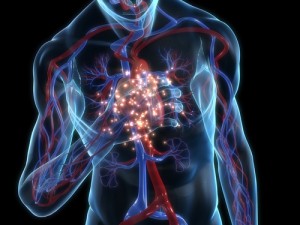
In the multi-center study, the researchers addressed the incidence of Supraventricular Arrhythmias (SVA) and risk factors, clinical manifestation, management, and impact on survival in 280 patients with Idiopathic Pulmonary Arterial Hypertension (IPAH), a condition in which the blood pressure in the pulmonary artery is increased, over 6 years. The patients enrolled in the study were on average 39 years old, and 40 of the patients had at least one SVA episode during an average 31 months of follow-up, leading to a 6-year frequency of 15.8%. Survival was significantly poorer in patients who developed SVAs than those who did not, with 1-year rates of 85% versus 92% and 6-year rates of 53% versus 75%. The most common SVAs experienced by the patients in the study were atrial fibrillation, heart flutter, and tachycardia.
[adrotate group=”4″]
Through the use of an electrocardiogram, restoration of the normal beating of the heart, known as sinus rhythm, was observed after treatment in all cases of atrial tachycardia, in less than half of atrial flutter, and in a quarter of atrial fibrillation cases. The survival of patients with transient SVAs was not significantly different from those without arrhythmias. On the other hand, the decrease in survival was confined to patients with persistent arrhythmia, a risk factor that increased mortality probability almost five times more after taking into account for possible confounders.
Importantly, the authors found that biomarkers such as heart enlargement, i.e. increased right ventricular diameter and left atrial area, mean right atrial pressure, and pulmonary vascular resistance were high risk factors for developing an SVA.
“These findings support that restoration and maintenance of sinus rhythm are important treatment goal[s] in IPAH patients,” wrote Dr. Jing and co-authors. “Thus, electrocardiogram (even Holter monitor), echocardiography and right heart catheterization should be part of our routine assessment for PAH patients.”