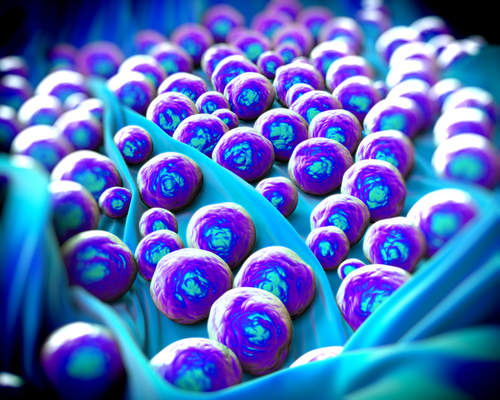
 A new study from a team of researchers of the University of Pittsburgh Center for Vaccine Research (CVR), entitled “Engineered Cationic Antimicrobial Peptides (eCAPs) to Overcome Multidrug Resistance by ESKAPE Pathogens” demonstrated the effectiveness of a new antibiotic alternative as an inhibitor of the growth of drug-resistant bacteria. The findings could someday impact the Cystic Fibrosis patient population in particular, who rely on viable anti-bacterial drugs to combat potentially deadly lung infections.
A new study from a team of researchers of the University of Pittsburgh Center for Vaccine Research (CVR), entitled “Engineered Cationic Antimicrobial Peptides (eCAPs) to Overcome Multidrug Resistance by ESKAPE Pathogens” demonstrated the effectiveness of a new antibiotic alternative as an inhibitor of the growth of drug-resistant bacteria. The findings could someday impact the Cystic Fibrosis patient population in particular, who rely on viable anti-bacterial drugs to combat potentially deadly lung infections.
Multiple drug resistance constitutes a threat to medical achievements, with estimates that in the U.S. at least 2 million people are infected with drug-resistant bacteria. For those with CF, who are often prescribed antibiotics on an ongoing basis to neutralize bacterial lung infections before they crop up, this issue is even more critical. However, in spite of these serious unmet medical needs, research into the development of new antibiotics that can fight bacteria resistance mechanisms have been scarce in the last decades.
“Very few, if any, medical discoveries have had a larger impact on modern medicine than the discovery and development of antibiotics,” said Dr. Ronald C. Montelaro in a recent press release. “However, the success of these medical achievements is being threatened due to increasing frequency of antibiotic resistance. It is critical that we move forward with development of new defenses against the drug-resistant bacteria that threaten the lives of our most vulnerable patients.”
In the study published in the journal Antimicrobial Agents and Chemotherapy, the team of researchers led by Ronald C. Montelaro, Ph.D., professor and co-director of Pitt’s CVR, developed two cationic antibiotic peptides (eCAPs), called WLBU2 and WR12 to overcome resistance from 143 clinical isolates representing the most common pathogens.
[adrotate group=”3″]
They compared the effects of common drugs (a natural antimicrobial peptide called LL37, and a standard antibiotic called colistin) and eCPAs. Results revealed that LL37 and colistin inhibited the growth of 51% the clinical isolates, whereas eCAPs inhibited 87% to 91%. Furthermore, bacteria treated with common drugs developed resistance in three days, while the same bacteria treated with the two eCAPs developed resistance only after 25 to 30 days. Furthermore, the two eCPAs (WLBU2 and WR12) were found to kill Pseudomonas aeruginosa after their resistance to the common compounds.
In the press release, Dr. Motelaro said about the performance of the eCPAs, “We were very impressed with the performance of the eCAPs when compared with some of the best existing drugs, including a natural antimicrobial peptide made by Mother Nature and an antibiotic of last resort. However, we still needed to know how long the eCAPs would be effective before the bacteria develop resistance.”
“We plan to continue developing the eCAPs in the lab and in animal models, with the intention of creating the least-toxic and most effective version possible so we can move them to clinical trials and help patients who have exhausted existing antibiotic options,” said Dr. Montelaro in the press release.
This study offers encouraging results, but requires further investigations of eCAPs for use in clinical settings.