A recent study entitled “Transcriptome meta-analysis of lung cancer reveals recurrent aberrations in NRG1 and Hippo pathway genes” reports worse outcomes for lung cancer patients with higher incidence of gene fusions. The study was published in the journal Nature Communications.
A recent study entitled “Transcriptome meta-analysis of lung cancer reveals recurrent aberrations in NRG1 and Hippo pathway genes” reports worse outcomes for lung cancer patients with higher incidence of gene fusions. The study was published in the journal Nature Communications.
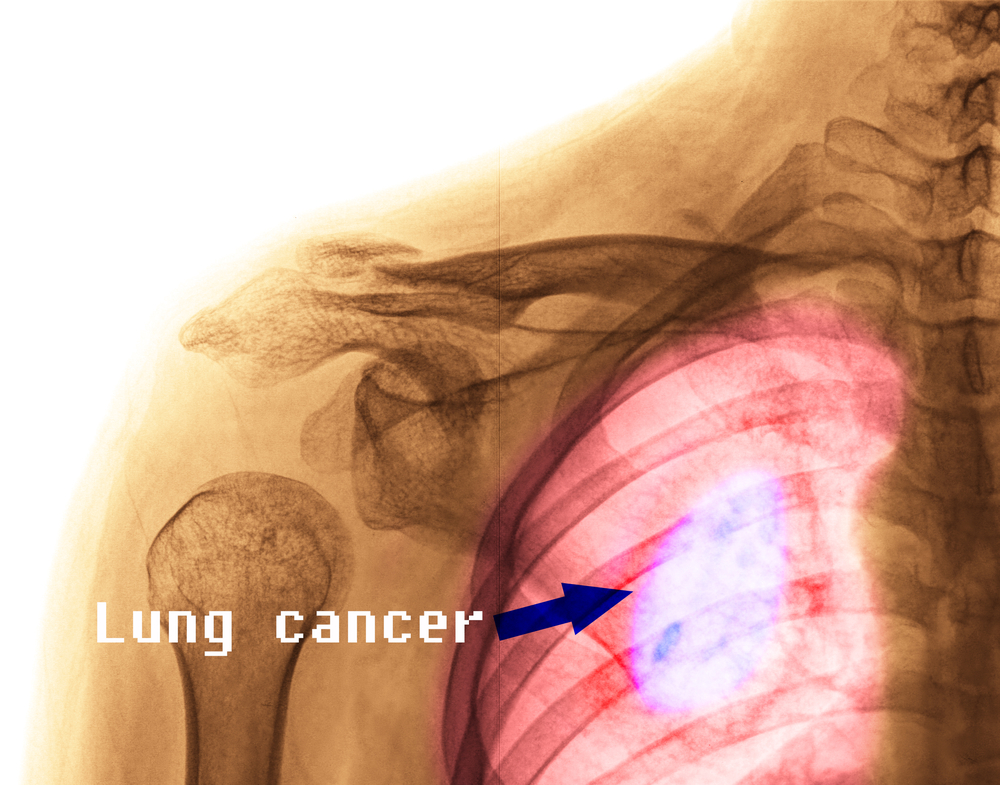
Lung cancer is the leading cause of death in both men and women cancer patients, with approximately 224,210 new cases diagnosed in 2014. While in some lung cancer subtypes several mutations were identified in key oncogenes, such as KRAS, EGFR, ALK and MET, thus empowering tumors with increasing tumorigenic potential, other genetic anomalies have still yet to be identified.
A team of researchers at the University of Michigan Comprehensive Cancer Center performed a meta-analysis on transcriptome data from 753 lung cancer samples, belonging to both smokers and non-smokers patients – 153 samples were obtained at the University of Michigan, 521 samples from the Cancer Genome Atlas, and the other 79 samples were retrieved from a recent published report. The authors were particularly interested in characterizing the gene fusion landscape of these tumors, since this process (characterized by the formation of a hybrid gene, composed of two previous separated genes) is known to impact cancer initiation and progression.
The researchers found a highly diverse gene fusion landscape in the profiled lung cancers. Specifically, they identified 6,348 unique fusions, occurring at a rate of approximately 13 fusions per sample. Their functional analysis pin-pointed gene fusions occurring in genes belonging to two pathways — the Hippo pathway, a well-known pathway that regulates tissue growth and cellular proliferation, and has been suggested to play a role in cancer; and the NRG1 gene pathway. Notably, the researchers found that these gene fusions occur without the occurrence of driver mutations, i.e., mutations that confer a selective advantage to the carrying cell.
The authors’ findings showed that an increasing number of gene fusions in a sample is associated with a poorer prognosis for lung cancer, therefore, the authors suggest this feature can work as an independent prognostic factor for patients’ survival.
[adrotate group=”3″]
The fusions in the Hippo pathway were identified in 3%, while NRG1 fusions in 4% of the lung cancer patients analyzed, thus targeted therapies against these factors can be potential successful therapeutics for these lung cancer patients.
Arul Chinnaiyan, M.D., Ph.D., director of the Michigan Center for Translational Pathology and S.P. Hicks Professor of Pathology at the University of Michigan Medical School noted, “We’ve previously had success in targeting therapies against low-recurrence gene fusions. Large-scale genome analyses like this allow us to identify more of the key drivers of each patient’s tumor so that we can match the most appropriate therapies.”