Research teams at the University of North Carolina at Chapel Hill and North Carolina State University report the discovery of a novel approach to inhalable vaccine creation through employing nanoparticles showing particular promise for targeting lung-specific respiratory diseases like influenza, pneumonia and tuberculosis.
 A study led by Dr. Catherine Fromen and Gregory Robbins, members of the DeSimone and Ting labs at UNC respectively, reveals that the surface charge of a particle plays a key role in eliciting immune responses in the lung. Using the Particle Replication in Nonwetting Templates (PRINT) technology invented in the DeSimone lab (see more detail about the PRINT process below). Dr. Fromen and Mr.
A study led by Dr. Catherine Fromen and Gregory Robbins, members of the DeSimone and Ting labs at UNC respectively, reveals that the surface charge of a particle plays a key role in eliciting immune responses in the lung. Using the Particle Replication in Nonwetting Templates (PRINT) technology invented in the DeSimone lab (see more detail about the PRINT process below). Dr. Fromen and Mr.  Robbins and their research colleagues were able to modify the specific surface charge of protein-loaded particles without disrupting of other particle characteristics, thus demonstrating the PRINT technology’s unique capacity to independently modify particle attributes in isolation.
Robbins and their research colleagues were able to modify the specific surface charge of protein-loaded particles without disrupting of other particle characteristics, thus demonstrating the PRINT technology’s unique capacity to independently modify particle attributes in isolation.
Particles with a positive surface charge were shown when delivered through the lung to induce both local and systemic antibody responses in the body, while by contrast, similarly composed particles with a negative surface charge were associated with weaker, in some instances undetectable, immune response stimulation, which suggests that particle charge is an important factor to consider in the context of pulmonary vaccination.
The research team’s findings, published in the Proceedings of the National Academy of Sciences, also have general public health implications for improving vaccine accessibility. For example, development of inhalable vaccines could potentially eliminate the need for vaccine refrigeration, not only extending shelf life, but also enabling vaccine distribution to low-resource areas, including in many developing countries that have dire need for better vaccine access.
The PNAS paper, entitled “Controlled analysis of nanoparticle charge on mucosal and systemic antibody responses following pulmonary immunization“ (Published online before print PNAS December 29, 2014, doi: 10.1073/pnas.1422923112) is coauthored by Catherine A. Fromen, Gregory R. Robbins, Tammy W. Shend, Marc P. Kaia, Jenny P. Y. Ting, and Joseph M. DeSimone, all associated with various departments at North Carolina State University, Raleigh, NC.
The researchers note that to their knowledge, “no other nano-based vaccine delivery platform has directly assessed the effects of nanoparticle charge on pulmonary vaccination without affecting other physio/chemical particle characteristics and/or antigen loading,” and that “The Particle Replication in Non-Wetting Templates nanoparticle fabrication process is unique in that it allows for isolation of charge as the sole variable in these studies while maintaining all other physical and chemical parameters constant.”
[adrotate group=”3″]
The coauthors observe that they found the positively charged nanoparticles instrumental in inducing robust mucosal and systemic antibody responses in the lungs, while negatively charged nanoparticles fail to do so — results that underscore that taking nanoparticle charge into consideration as a critical design parameter in development of vaccines for pulmonary-based diseases may also have similar implications for particulate vaccination through other routes of administration.
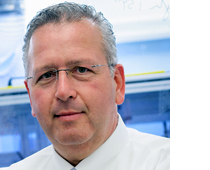 Joseph DeSimone is Chancellors Eminent Professor of Chemistry at UNC, whose lab’s focus is on applying computer generated lithographic fabrication technologies for design and synthesis of new medicines and vaccines; Nanomedicine; Interventional oncology; Medical devices; Inhalable therapeutics; Fluoropolymers: photolithography, fuel cells, microfluidics, minimally adhesive surfaces; Colloid, surfactant and surface chemistry; Patterning surfaces, manipulation of light; Polymer synthesis and processing in carbon dioxide: new polymers, interfacial science and colloids, reaction kinetics and engineering, green chemistry; and Process engineering.
Joseph DeSimone is Chancellors Eminent Professor of Chemistry at UNC, whose lab’s focus is on applying computer generated lithographic fabrication technologies for design and synthesis of new medicines and vaccines; Nanomedicine; Interventional oncology; Medical devices; Inhalable therapeutics; Fluoropolymers: photolithography, fuel cells, microfluidics, minimally adhesive surfaces; Colloid, surfactant and surface chemistry; Patterning surfaces, manipulation of light; Polymer synthesis and processing in carbon dioxide: new polymers, interfacial science and colloids, reaction kinetics and engineering, green chemistry; and Process engineering.
Recent breakthroughs in the DeSimone laboratories using specifically-designed materials for imprint or soft lithography have enabled an extremely versatile and flexible method for the direct fabrication and harvesting of monodisperse, shape-specific nano-biomaterials. The method, referred to as Particle Replication In Non-wetting Templates, or PRINT, allows for the fabrication of monodisperse particles with simultaneous control over structure (i.e. shape, size, composition) and function (i.e. cargo, surface structure).
The lab notes that unlike other particle fabrication techniques, PRINT is delicate and general enough to be compatible with a variety of medical applications. The capability of simultaneously changing a nanoparticle’s size, shape, and surface properties as well as its chemical composition is a unique attribute of the PRINT process, and manipulating these physical properties can increase the therapeutic effectiveness of a drug, as well as reduce side effects and improve patient compliance.
The DeSimone lab is investigating various routes by which to administer PRINT particles, noting that improved drug delivery to the lungs via inhalation represents a promising innovation in treating many pulmonary and systemic diseases. By controlling particle size, shape and composition, PRINT-developed aerosol-delivered medicines offer improved dose uniformity, and with that platform, the DeSimone group is investigating effects of particle shape on powder entrainment and airway deposition, and opportunities for specific targeting or de-targeting of airway macrophages.
PRINT particles are also being investigated as to co-delivery media for antigens and adjuvants administered as highly effective particulate vaccines, the DeSimone researchers noting that micro and nano-sized particles show great potential in vaccine development both as vaccine carriers and particulate adjuvants.
 Dr. Jenny Ting is William Rand Kenan Professor of Microbiology and Immunology in UNCs School of Medicine, Co-Director, Inflammatory Diseases Institute, Director, Center for Translational Immunology, Program Leader at the Lineberger Comprehensive Cancer Center, and also on the UCRF Program Planning Committee. The Ting lab has broad interest in application of cutting edge ideas and technology to study of disease-relevant issues. The lab’s current major research foci include innate immunity, dendritic cell function, cell death, autophagy, signal transduction, gene discovery, functional genomics and proteomics, nanoparticles, gene regulation, neuro-inflammation and microglial cells. Clinical issues of interest include multiple sclerosis, cancer, autoimmune diseases, biologic therapy, infection and inflammation.
Dr. Jenny Ting is William Rand Kenan Professor of Microbiology and Immunology in UNCs School of Medicine, Co-Director, Inflammatory Diseases Institute, Director, Center for Translational Immunology, Program Leader at the Lineberger Comprehensive Cancer Center, and also on the UCRF Program Planning Committee. The Ting lab has broad interest in application of cutting edge ideas and technology to study of disease-relevant issues. The lab’s current major research foci include innate immunity, dendritic cell function, cell death, autophagy, signal transduction, gene discovery, functional genomics and proteomics, nanoparticles, gene regulation, neuro-inflammation and microglial cells. Clinical issues of interest include multiple sclerosis, cancer, autoimmune diseases, biologic therapy, infection and inflammation.
This research is supported by the National Institute of Allergy and Infectious Diseases-funded Center for Translational Research as well as the Defense Threat Reduction Agency.
Sources:
University of North Carolina at Chapel Hill
North Carolina State University
Proceedings of the National Academy of Sciences
Image Credits:
University of North Carolina at Chapel Hill