A recent study published in the journal Rheumatology revealed that a high systolic pulmonary artery pressure (sPAP) can elevate the mortality risk in individuals with systemic sclerosis (SSc).
A recent study published in the journal Rheumatology revealed that a high systolic pulmonary artery pressure (sPAP) can elevate the mortality risk in individuals with systemic sclerosis (SSc).
SSc is a rare, chronic connective tissue disease, characterized by increased fibroblast activity which results in abnormal growth of connective tissue and thickening of the skin. It is a disorder more common among women and it has two forms: limited cutaneous, which is restricted to the skin on the face, hands and feet, and diffuse cutaneous that has the risk of progressing to visceral organs such as the lungs.
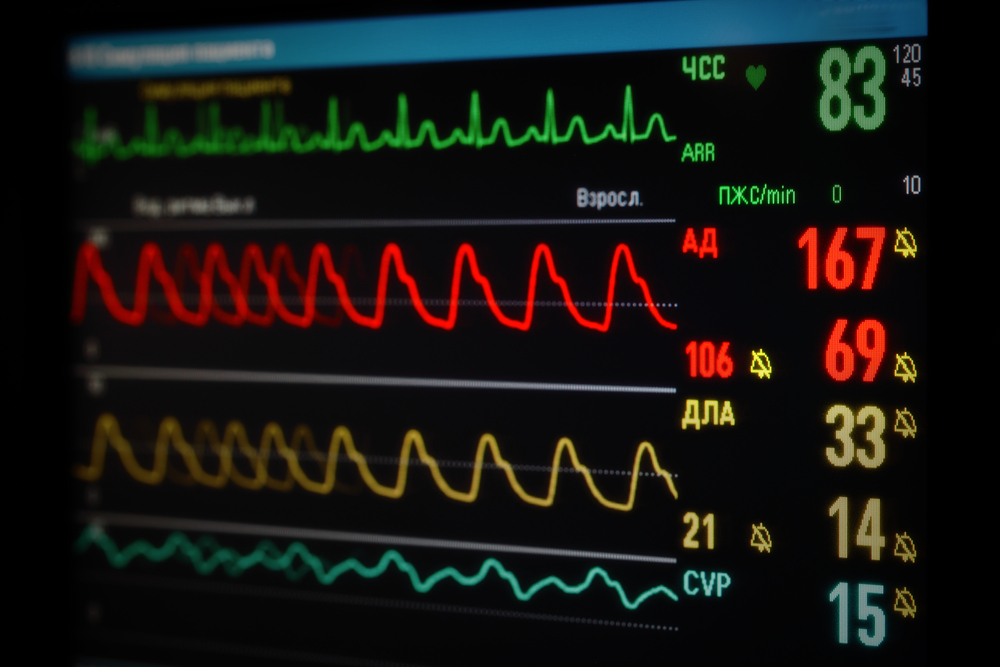
Pulmonary arterial hypertension corresponds to an increase of blood pressure in the arteries that supply blood to the lungs, the pulmonary arteries. It is a life-threatening condition and a common complication of SSc, being considered one of the leading causes of death in SSc patients.
The study, entitled “Value of systolic pulmonary arterial pressure as a prognostic factor of death in the systemic sclerosis EUSTAR population,” was based on data from the European League Against Rheumatism Scleroderma Trial and Research (EUSTAR) database. Data was collected from 1,476 SSc patients between January 2005 and December 2011. All patients had been subjected to an echocardiography, which is the screening tool most used to assess pulmonary hypertension in SSc patients. The mean duration of the follow-up study was two years. The data obtained also comprised information regarding disease symptoms, renal crisis history and comorbidities. 87% of the patients studied were females, with a mean age of 56.3 years and 31% had diffuse SSc.
[adrotate group=”4″]
The researchers found that the hazard ratio (HR) for death was 1.67, 2.37, 3.72 and 9.75 considering sPAP indexes between 30 – 36 mmHg, 36 – 40 mmHg, 40 – 50 mmHg and higher than 50 mmHg, respectively. In terms of survival prognostic factor, the best cut-off for sPAP was found to be 36 mmHg, where an estimated sPAP equal or higher than this value at baseline echocardiography was associated with a reduced survival in SSc patients.
The team proposes that sPAP should be considered as an additional independent survival prognostic factor, and that sPAP levels that equal or higher than 36 mmHg should be interpreted as a red flag indicating a high mortality risk in SSc patients.