 Researchers at the VU University Medical Center in Amsterdam, The Netherlands recently published findings in The International Journal of Cardiovascular Imaging that reveal specific measurements obtained by standard computed tomography pulmonary angiography (CTPA) can be used as an accurate predictive tool for pulmonary hypertension. The study is entitled “Predicting pulmonary hypertension with standard computed tomography pulmonary angiography.”
Researchers at the VU University Medical Center in Amsterdam, The Netherlands recently published findings in The International Journal of Cardiovascular Imaging that reveal specific measurements obtained by standard computed tomography pulmonary angiography (CTPA) can be used as an accurate predictive tool for pulmonary hypertension. The study is entitled “Predicting pulmonary hypertension with standard computed tomography pulmonary angiography.”
Pulmonary hypertension corresponds to a cardiopulmonary disorder characterized by an abnormally high blood pressure in the blood vessels that supply the lungs (usually a mean pulmonary artery pressure above 25 mmHg). It is a life-threatening condition that can lead to difficulties in breathing and right-sided heart failure.
Pulmonary hypertension can be difficult to diagnose early due to the non-specific nature of the symptoms, such as fatigue and shortness of breath (dyspnea). An early diagnosis and subsequent treatment are known to improve patients’ clinical outcome, justifying the importance of having accurate screening tools for this disorder.
[adrotate group=”4″]
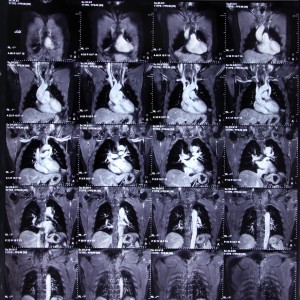
Pulmonary hypertension can be detected on a standard CTPA, which is usually performed in individuals presenting dyspnea. Patients with pulmonary hypertension frequently have an increased diameter-ratio of the pulmonary artery to the ascending aorta (PA/AA) that can be identified in a CTPA by an attentive radiologist.
The research team hypothesized that the CTPA diagnostic sensitivity for pulmonary hypertension can be improved by combining PA/AA measurements and information on the heart’s structure such as ventricular measurements. To test their hypothesis, researchers evaluated 51 patients with precapillary pulmonary hypertension who were submitted to CTPA and right heart catheterization (to assess the blood flow in the right side of the heart). As a control, 25 individuals without pulmonary hypertension also underwent both CTPA and right heart catheterization procedures.
Researchers found that a standard CTPA using only the PA/AA measurement had an accuracy of around 90.1% in discriminating patients with pulmonary hypertension from the ones without. When the ratio of the heart right ventricular and left ventricular diameter (RV/LV) was added to the PA/AA measurement, the accuracy of the diagnosis was improved to more than 98%. No significant differences were found between RV/LV measurements by either axial view or a manually reconstructed four chamber view.
The research team concluded that the CTPA predictive value for pulmonary hypertension is enhanced when ventricular and pulmonary artery measurements are combined and suggests that radiologists should assess both parameters when performing CTPA. A PA/AA ratio higher or equal to 1 or a RV/LV ratio higher or equal to 1.20 is indicative of pulmonary hypertension and the patient should be further examined to confirm the diagnosis.
Researchers emphasize that CTPA by itself should not be used as a primary screening tool for pulmonary hypertension, but rather as a predictive tool that requires further validation by suitable techniques that can confirm or rule out the disease, for instance by an echocardiography.

