Researchers at the Catholic University of Korea in Seoul reported that a portion of patients with systemic lupus erythematosus (SLE) may develop pulmonary hypertension, and propose a biomarker to diagnose the condition. The study was recently published in the International Journal of Rheumatic Diseases and is entitled “High levels of uric acid in systemic lupus erythematosus is associated with pulmonary hypertension.”
SLE is a severe autoimmune disease in which the body’s own immune system overreacts and attacks healthy joints and organs, resulting in inflammation, swelling, pain, disability and often in tissue destruction in multiple organs.
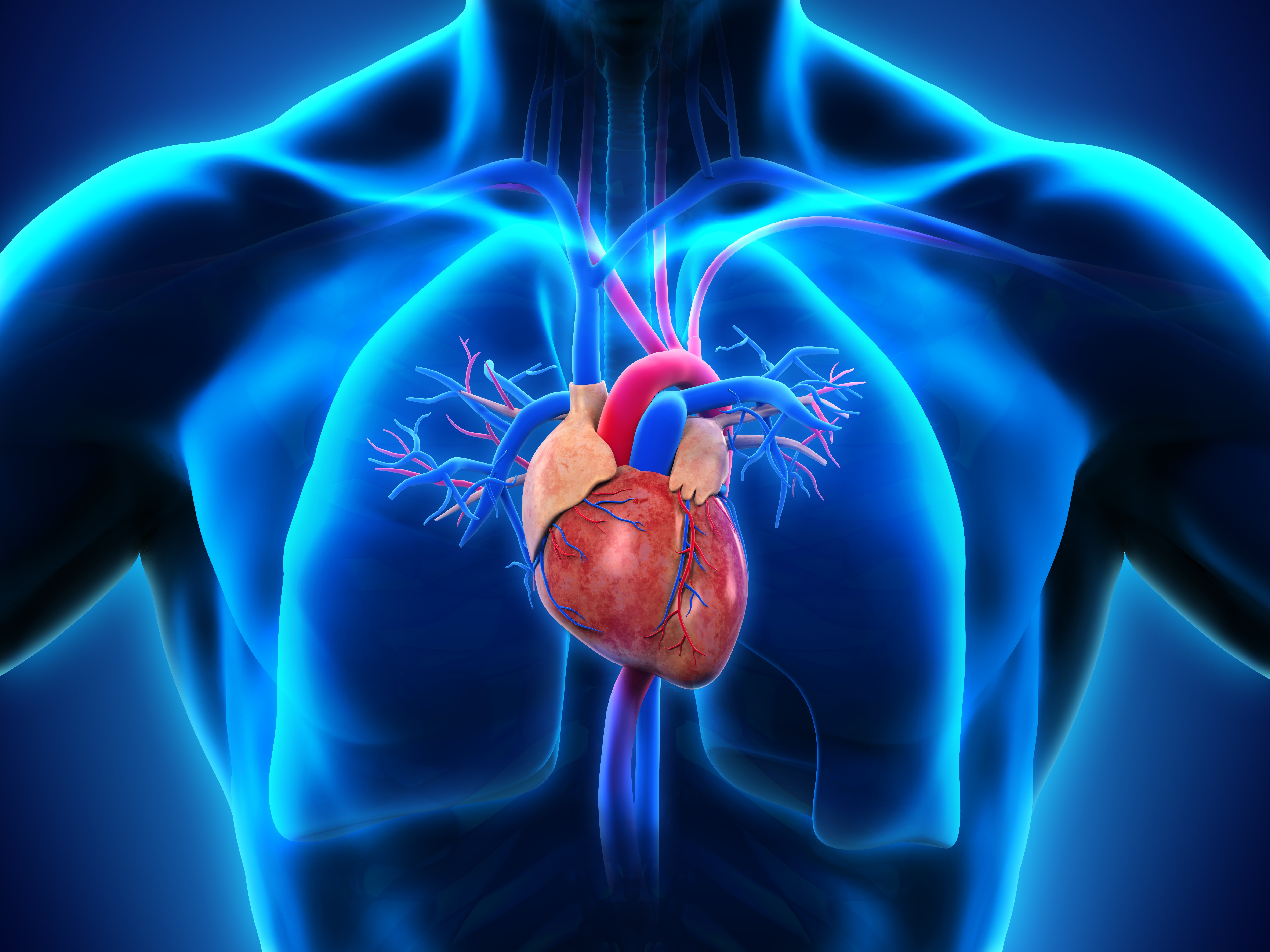
A rare, life-threatening cardiopulmonary complication of SLE is pulmonary hypertension, a debilitating condition characterized by abnormally high blood pressure in the pulmonary arteries that supply blood to the lungs, leading to vascular remodeling, difficulties in breathing, chest pain, right-sided heart failure and eventually death. An early diagnosis of pulmonary hypertension is critical to improve the clinical outcome in SLE patients.
The goal of the study was to estimate the prevalence of pulmonary hypertension and associated risk factors in SLE patients. Researchers conducted a prospective cross-sectional study with 114 SLE patients. The patients’ pulmonary arterial pressures were determined through non-invasive transthoracic echocardiography. The team established pulmonary hypertension as a resting systolic pulmonary artery pressure equal or higher than 40 mmHg, in the absence of left heart disease.
Researchers found that 7.8% of the SLE patients had pulmonary hypertension, and that their associated SLE disease activity score was higher. Serum uric acid was found to be significantly higher in SLE patients with pulmonary hypertension in comparison to those without the condition, and to correlate with the patient’ systolic pulmonary artery pressure. An excess of uric acid (hyperuricemia) is not common in SLE patients except in cases of renal insufficiency or the use of particular medication. The team believes that pulmonary hypertension might set up a favorable environment for the production of uric acid. Interestingly, researchers found that at a cutoff level of 6.5 mg/dL, serum uric acid had a reasonable accuracy as a predictor of pulmonary hypertension in SLE patients (sensitivity of 66.7% and specificity of 96.2%).
The team suggests that serum uric acid levels can be a useful indicator of pulmonary hypertension associated with SLE. “A significant number of SLE patients in rheumatology practice have undiagnosed PH with few discernible symptoms,” wrote the research team according to a news release. “Serum UA [uric acid] level may be useful as a surrogate marker for screening of PH in patients with SLE.”