In a recent study entitled “Changes of Proteases, Antiproteases, and Pathogens in Cystic Fibrosis Patients’ Upper and Lower Airways after IV-Antibiotic Therapy,” authors highlight the alterations in the balance between proteases/antiproteases (key factors in inflammation and tissue damage), and pathogen colonization, specifically Pseudomonas aeruginosa in Cystic Fibrosis patients who underwent antibiotic treatment. The study was published in the journal Mediators of Inflammation.
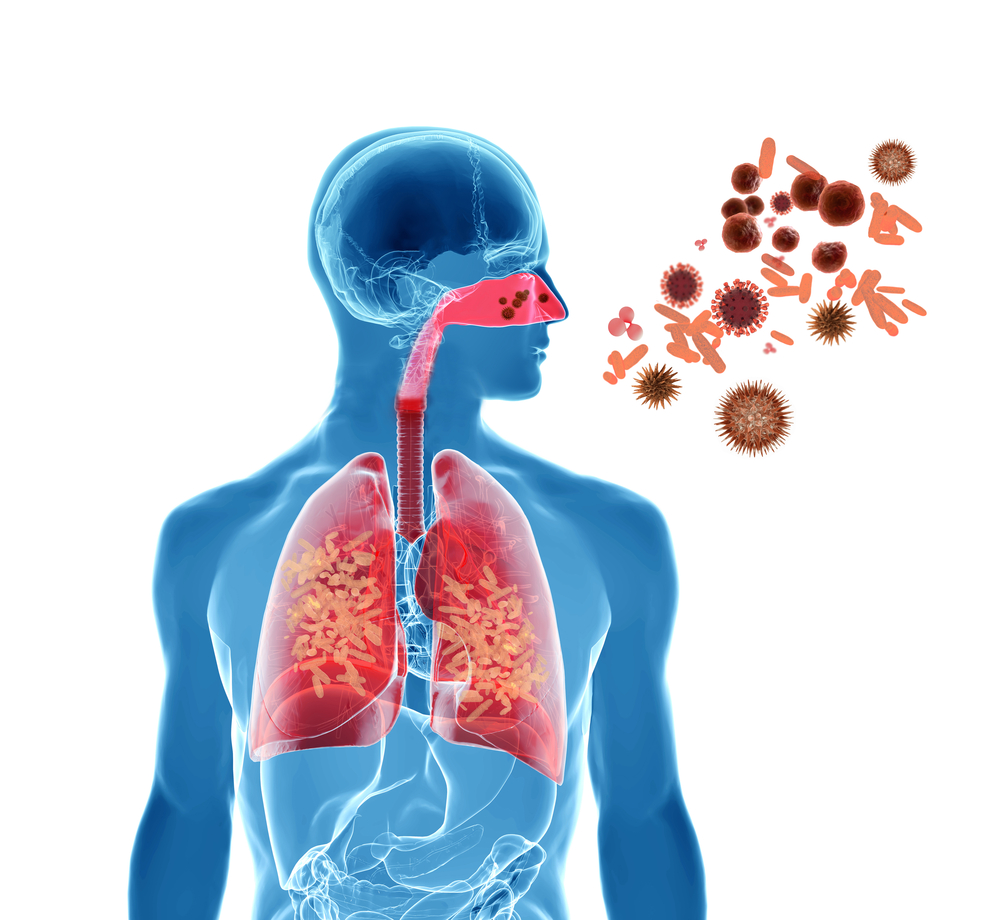
Cystic Fibrosis (CF) is caused by mutations in the Cftr gene (cystic fibrosis transmembrane conductance regulator gene). The disease is characterized by accumulation of thick mucus, particularly in the lungs, leading to recurrent infections that are associated with difficulties in breathing and culminating in patients’ death due to pulmonary failure. One of the most common pathogens colonizing both upper and lower airways of CF patients’ lungs is Pseudomonas aeruginosa –– it enhances pulmonary destruction by promoting the release of proteolytic enzymes. In fact, chronic inflammation in CF airways is caused by an imbalance of proteases and antiproteases.
In this new study, a team of researchers analyzed the alterations to pathogen colonization, proteases, antiproteases and inflammatory cells in CF patients’ upper (determined by nasal lavage) and lower airway (determined via sputum) compartments before and after intravenous- (IV-) antibiotic therapy. The study was conducted at the Jena University Hospital CF Center in Germany and enrolled 17 CF patients who were submitted to 19 IV-antibiotic treatments. The team observed that the upper airways harbor lower concentrations of proteases and antiproteases, as well as inflammatory cells, when compared to the lower airways. When analyzing the colonization by Pseudomonas aeruginosa in patients with a chronic colonization with this pathogen, authors observed that before and after antibiotic therapy Pseudomonas aeruginosa was present in upper and lower airways. This suggests that IV-antibiotic treatment may reduce Pseudomonas aeruginosa burden, but it fails to completely eliminate the pathogen from patients’ airways.
The authors highlight that while their study is the first to describe changes in proteases/antiproteases balance, together with pathogen colonization in upper and lower airways compartments in CF patients, future studies should extend the analysis to the paranasal sinuses (group of four paired air-filled spaces that surround the nasal cavity) in order to uncover how an imbalance in proteases/antiproteases affects the presence of pathogens in these regions.