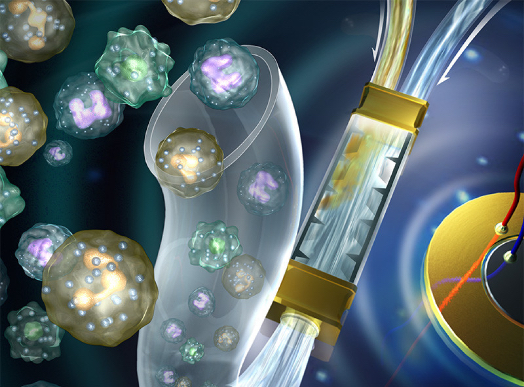
A device capable of using ultrasonics to mixing liquid developed at the Penn State Materials Research Institute is the first and most difficult component in a miniaturized system for low-cost sputum analysis of samples from patients with pulmonary diseases such as tuberculosis and asthma. The latter is a common disease affecting an estimated 300 million people worldwide. Asthma pathogenesis of involves airway inflammation, airway remodeling, and hyperreactivity, which lead to difficulty in breathing that can be deadly if not properly controlled.
Steroid medications can successfully treat asthma in most cases, but side-effects of long-term steroid administration can be profound, and in the approximately five percent of patients with severe refractory asthma, these medications fail to adequately control the disease.
The ultrasonic device, developed by engineers at Penn State in collaboration with researchers at the National Heart, Lung, and Blood Institute (NHLBI) , part of the National Institutes of Health, and the Washington University School of Medicine, will benefit patients in the U.S., where 12 percent of the population, or approximately 19 million people, have asthma, as well as in undeveloped regions where TB is still a widespread and often deadly contagion.
“To develop more accurate diagnosis and treatment approaches for patients with pulmonary diseases, we have to analyze sample cells directly from the lungs rather than by drawing blood,” says Penn State professor of engineering science and mechanics Tony Jun Huang. Dr. Huang with his research group are the inventors of this and other acoustofluidic devices based on ultrasonic waves. For instance, since various drugs are used to treat different types of asthma patients, knowing what a person’s immunophenotype is enables provision of personalized medicine for their particular disease.
There are several shortcomings and deficiencies with current standard methods of sputum analysis. Firstly, human biological specimens can be contagious, and sputum analysis requires handling of specimens in several discrete machines. By contrast with a lab on a chip device, all biospecimens remain safely contained with in a single disposable component.
Secondly, sample sizes required for analysis using current systems are often larger than a patient can easily produce. The acoustofluidic sputum liquefier created by Dr. Huang’s group requires a 100 times smaller sample while still providing accuracy equivalent to the standard system.
Thirdly, current systems are difficult to use and require trained operators, while with a lab on a chip system, a nurse can operate the device with a touch of a few buttons to obtain a readout, or the patient could even operate the device at home. In addition, the disposable portion of the device should cost less than a dollar to manufacture.
Po-Hsun Huang, a graduate student in the Huang group and the first author on the recent paper describing the device in the Royal Society of Chemistry journal Lab on a Chip, says: “This will offer quick analysis of samples without having to send them out to a centralized lab. While I have been working on the liquefaction component of the device, my lab mates are working on the flow cytometry analysis component, which should be ready soon. This is the first on-chip sputum liquefier anyone has developed.”
“This on-chip sputum liquefier is a significant advance regarding our goal of developing a point-of-care diagnostic device that will determine the type of inflammation present in the lungs of asthmatics,” says Stewart J. Levine, a Senior Investigator and Chief of the Laboratory of Asthma and Lung Inflammation in the Division of Intramural Research at NHLBI. “This will allow health care providers to individualize asthma treatments for each patient and advance the goal of bringing precision medicine into clinical practice. Dr. Levine’s lab is focused on developing new treatment approaches for patients with severe asthma.”
This research was supported by the American Asthma Foundation Scholar Award, the National Science Foundation, and the NHLBI Division of Intramural Research. Portions of this work were carried out in the Penn State Nanofabrication Facility, a node of the NSF-funded National Nanotechnology Infrastructure Network.
Sources:
Newsroom: Penn State Materials Research Institute
Lab on a Chip
Image Credits:
Penn State