A new study recently published in the journal Proceedings of the National Academy of Sciences (PNAS) revealed a new DNA nanoparticle that can cross the lung mucus barrier representing a promising vehicle for gene therapy in several lung disorders. The study is entitled “Highly compacted biodegradable DNA nanoparticles capable of overcoming the mucus barrier for inhaled lung gene therapy” and was conducted by researchers at the Johns Hopkins University School of Medicine and Johns Hopkins University in the United States, and Federal University of Rio de Janeiro in Brazil.
Nanotechnology is defined by the employment of nanoparticles at supramolecular levels. This technology has allowed significant advances in the medical field, namely on drug development and targeted delivery. The use of synthetic nanoparticle-based gene delivery systems is increasing as it offers a highly tunable method to deliver therapeutic genes.
In the case of the respiratory system, the use of nanoparticles poses a challenge as these have to overcome biological barriers to properly deliver the therapeutic genes. The mucus barrier in the lungs protects the organ from injury or infection caused by foreign substances and microbes; however, this natural protective mechanism also prevents several inhaled therapeutics to reach their target, the lung epithelium underlying the mucus layer.
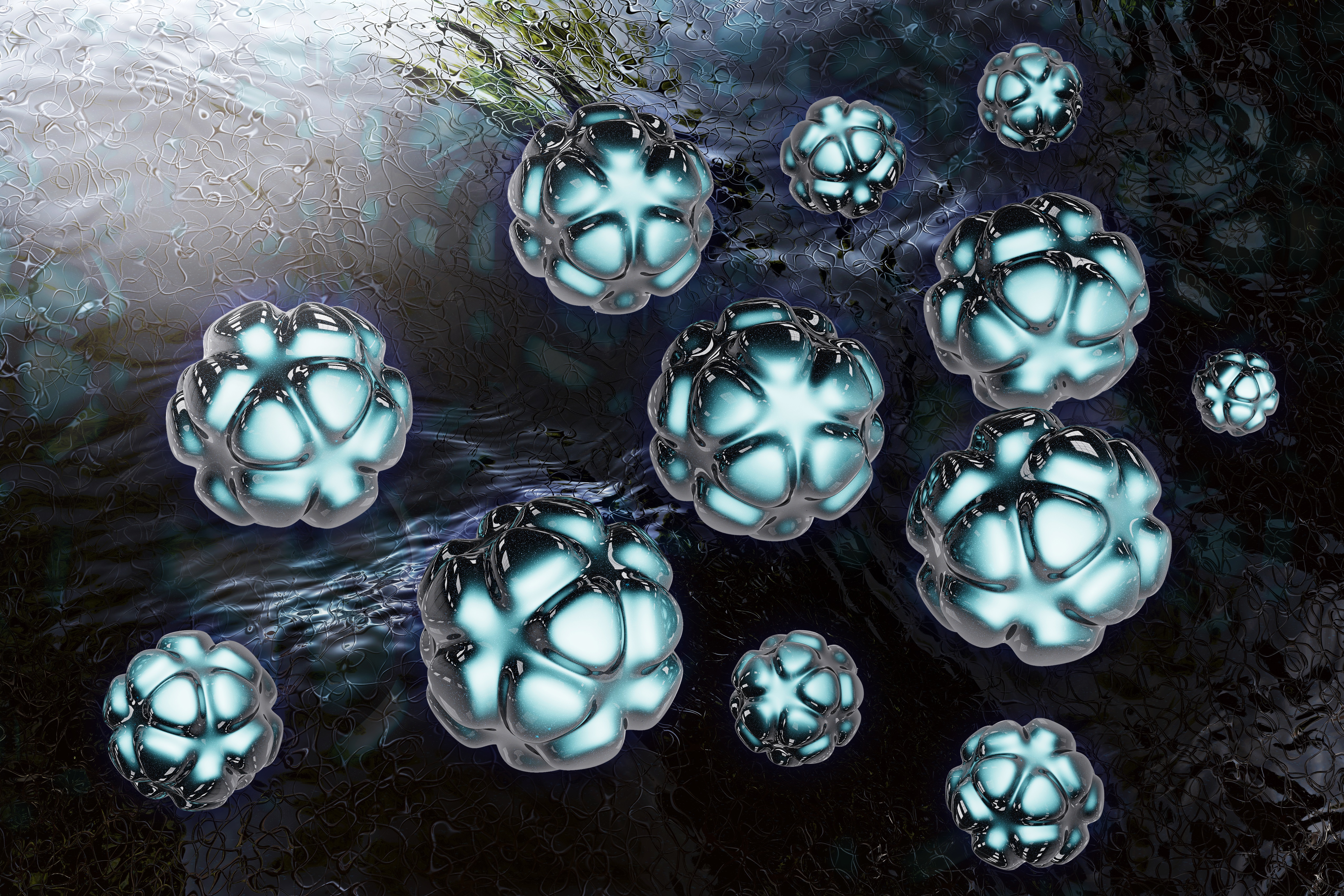
Researchers have now developed a DNA-loaded nanoparticle able to cross the mucus barrier in the lung airways. These particular nanoparticles are highly stable and based on innovative biodegradable polymers — poly(β-amino esters) (PBAEs), coated with a non-sticky polymer called polyethylene glycol. These nanoparticles were found to efficiently penetrate the human airway mucus layer. In mouse models, the PBAE-based mucus-penetrating DNA nanoparticles were found to provide a high, robust expression level of the therapeutic gene delivered in the animal’s lungs for at least four months after a single administration; an expression found to be superior to several other gene delivery systems including non-viral platforms. In terms of safety, the nanoparticles exhibited a safe profile with no signs of toxicity being reported after intratracheal administration. In addition, the research team designed this delivery system in a way that it is completely biodegradable, so it does not accumulate within the body.
“To our knowledge, this is the first biodegradable gene delivery system that efficiently penetrates the human airway mucus barrier of lung tissue,” said the study’s senior author Dr. Jung Soo Suk in a press release. “With one dose, you can get gene expression — i.e., production of therapeutic proteins — for several months.”
These new findings are especially important for cystic fibrosis (CF), a life-threatening genetic disease in which a defective gene, called cystic fibrosis transmembrane conductance regulator (CFTR), causes the body to form unusually thick, sticky mucus that can result in serious respiratory and gastrointestinal manifestations. In the study, the team showed that the delivery of normal copies of the CFTR gene through their mucus-penetrating DNA-loaded nanoparticles could mediate the production of functional proteins in the long-term.
The research team concluded that the DNA-loaded nanoparticles developed are the first gene delivery system that is efficiently able to penetrate the human airway mucus barrier, having an excellent safety profile. The team believes that their new approach for inhaled gene therapy opens the possibility of directly delivering therapeutic genes to the lungs in levels that are effective for the treatment of several life-threatening lung disorders including cystic fibrosis, chronic obstructive pulmonary disease (COPD) and asthma. One major advantage of this system emphasized by the authors is the fact that since a single dose might theoretically last for several months, patients would most likely experience less adverse effects in comparison to therapies based on prolonged, regular drug administration. The team is, however, cautious and suggests that further studies should confirm their results and eventually optimize the system for clinical use in humans.