In a new study entitled “Unraveling the Pathophysiology of the Asthma-COPD Overlap Syndrome: Unsuspected Mild Centrilobular Emphysema Is Responsible for Loss of Lung Elastic Recoil in Never Smokers With Asthma With Persistent Expiratory Airflow Limitation,” the authors report a new observation in nonsmoker patients with asthma-COPD overlap syndrome and underscore the need for additional and intensive studies to unravel the complete pathophysiology associated with asthma-COPD overlap syndrome. The study was published in the journal CHEST.
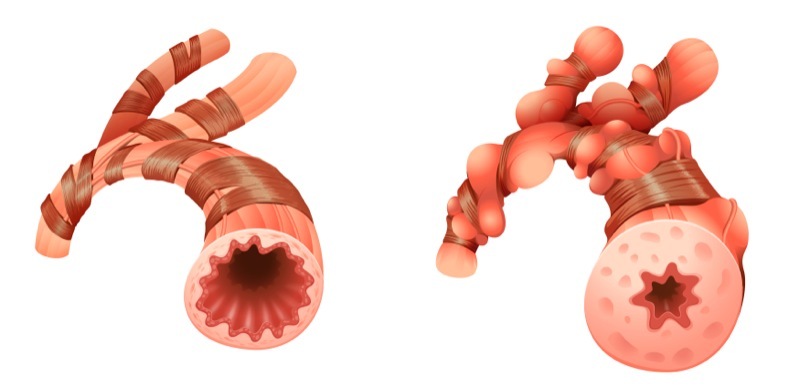
Asthma-COPD overlap syndrome (ACOS) accounts for 15 to 25% of obstructive airway diseases and patients affected with ACOS usually exhibit worse symptoms and clinical outcomes when compared to patients with asthma or chronic obstructive pulmonary disease (COPD) alone. ACOS syndrome is not well recognized, since it is difficult to separate asthma from COPD due to the overlapping symptoms of both diseases. Currently, ACOS patients are defined as smokers that exhibit chronic expiratory airflow obstruction despite treatment, and experience both symptoms of asthma and COPD. The authors in this new study, however, report that a small group of treated nonsmokers also exhibit moderate to severe asthma with limiting expiratory airflow, although they may experience some symptom reversibility. ACOS is believed to occur as the result of lung airway remodeling, especially in small airways.
Authors of the study highlight that they observed reversible loss of elastic recoil in the lung and persistent expiratory airflow limitation in nonsmoking patients with ACOS. Notably, however, the causes behind these phenotypes remain unknown.
In the study, the researchers noted a new observation made among 10 treated patients who never smoked and have asthma with persistent expiratory airflow obstruction. They observed that all patients had a significant decrease in lung elastic recoil, but also microscopic mild centrilobular, i.e., primarily in the upper lobes, and emphysema (the most common morphological subtype of pulmonary emphysema, a long-term, progressive lung disease leading to shortness of breath due to gradual damages in lungs alveoli).
As a result of this observation, the authors highlight that these findings are of particular importance and demonstrate the need to perform further studies and confirm the pathophysiologic observations to discover if indeed they are markers of ACOS. The research team also suggests that these potential ACOS alterations may be due to proinflammatory and proteolytic signaling cascades, which remains currently unaddressed.