Researchers at The Scripps Research Institute recently found that the mutated cystic fibrosis transmembrane conductance regulator (CFTR) protein found in many cystic fibrorsis patients interacts with wrong neighboring proteins, and these interactions block its correct function. The study, titled “∆F508 CFTR interactome remodelling promotes rescue of cystic fibrosis,” was published in Nature.
Cystic fibrosis (CF) is a hereditary disease that affects the lungs and digestive system, most frequently caused by a mutation in the cystic fibrosis gene known as F508del, leading to the incorrect folding and processing of CFTR in cells. CFTR is normally found at the cell surface and is necessary for the proper movement of sodium and chloride (salt) in and out of cells. This process is crucial for the correct hydration of the lungs, intestine, and pancreas. There is no cure for this condition and the standard therapy aims to control — rather than treat — its symptoms.
Previous studies have shown that mutated CFTR recovers its functions at low temperatures. As a result, the research team believes that a better understanding of the CFTR protein may be crucial for the development of new therapies.
“[T]he idea behind our new study was to find new drug candidates that could mimic what we see at low temperatures,” said Sandra Pankow, co-first author of the study, in a press release.
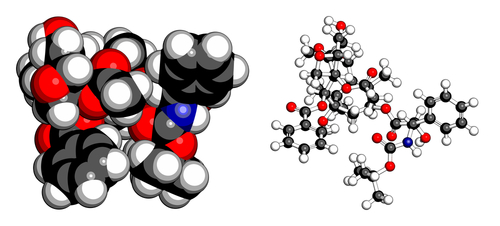
The research team developed a new method to identify proteins and analyze data called Co-Purifying Protein Identification Technology (CoPIT). With this tool, the researchers were able to identify almost all the proteins CFTR interacted with — even the secondary and tertiary protein interactions. They performed the first comprehensive analysis of ∆F508 CFTR interactions with other proteins, and its dynamics during temperature change and inhibition of histone deacetylases, enzymes that play essential roles in regulating gene transcription. Notably, these enzymes have been suggested as potential therapeutic targets for fibrotic disorders.
During the analysis, the researchers were surprised to find that the ΔF508 CFTR mutant acquired a completely novel “disease-specific” interaction network. “The proteins and the interactions we’ve identified really fuel the pipeline for new drug targets to treat cystic fibrosis,” said Casimir Bamberger, co-first author of the study.
Pankow said they identified 300 proteins that had changed their level of interaction and, in addition, 200 more proteins interacted with the mutated CFTR.
The research team limited their analysis to eight key disruptive proteins that interacted with the mutated CFTR and interfered with its function. They used a gene silencing strategy to remove or “knock-down” those proteins, and inhibit the interaction between them and ΔF508 CFTR. They found that without the additional interactions, ΔF508 CFTR partially recovered its normal function.
The authors say these findings may be an important step in the development of therapies that target the origin of cystic fibrosis and not just its symptoms.
The researchers now plan to search for small molecule drug candidates that might target these disruptive proteins. Importantly, they also have released their raw CoPIT data so other scientists might explore the clinical implications of CFTR interactions.