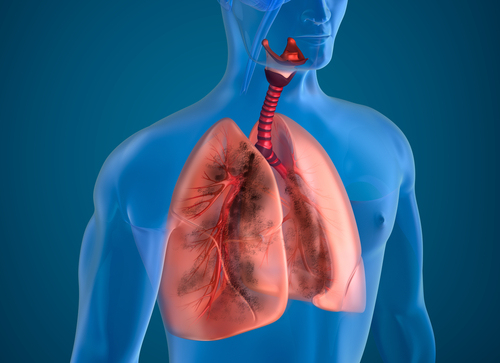
Airway clearance therapy (ACT) is an important treatment approach for patients with impaired ciliary function or other difficulties in clearing the lungs of mucus and harmful particles. Evidence indicates that ACT minimizes the effects of lung obstructions in afflicted patients, as discussed in the review article, “Airway Clearance Therapy: Finding the Evidence.”
Many different types of ACT are in use, including breathing techniques, postural drainage, positive expiratory pressure (PEP) mechanical devices, and high-frequency chest wall oscillation (HFCWO), also known as high-frequency chest compression (HFCC). Patients are treated with HFCWO using special inflatable vests that apply cyclical pressure at a frequency between 2 and 25 times per second (Hz). The oscillations are intended to break up and mobilize airway secretions, making it easier for the patients to rid their lungs of obstructions. Often, patients with cystic fibrosis are treated with HFCWO, as reported by Cystic Fibrosis News Today, but a host of other lung diseases also benefit from the treatment. A number of studies further show this treatment might be preferred by patients.
Another condition successfully treated by HFCWO is bronchiectasis, a disease in which the bronchi are inflamed. A study of 37 patients, entitled “Effectiveness of Treatment with High-Frequency Chest Wall Oscillation in Patients with Bronchiectasis,” identified that patients significantly improved their functional respiratory tests following treatment with HFWCO. The results for HFCWO-treated patients were just as sufficient as those from patients treated with traditional chest physiotherapy, indicating that bronchiectasis patients who need daily airway clearance may want to use HFCWO vests.
Treating primary ciliary dyskinesia (PCD) is another use for HFCWO vests, in addition to its more common applications in helping patients with cystic fibrosis and non-cystic fibrosis bronchiectasis. In PCD, patients’ cilia in the lungs are dysfunctional and cannot clear mucus, bacteria, or other particles from the lungs, according to Genetics Home Reference. To help adolescent patients with PCD, a group of researchers from Marmara University School of Medicine in Istanbul, Turkey, sought to compare HFCWO, postural drainage, and conventional cardiopulmonary respiration (CPR) in the journal article “Comparison of Conventional Pulmonary Rehabilitation and High-Frequency Chest Wall Oscillation in Primary Ciliary Dyskinesia.”
The outcomes for assessment were changes in forced vital capacity (FVC), forced expiratory volume in one-second (FEV1), forced expiratory flow (FEF), and peak expiratory flow (PEF). Between HFCWO and CPR, there were no significant differences — each allowed pulmonary function to increase significantly. Yet when comfort was considered, patients preferred HFCWO therapy administered at home to CPR administered at the hospital. This suggests that patients who do not adhere to CPR may do well on HFCWO.
Other new applications for HFCWO are being studied. For example, “A Pilot Study of the Impact of High-Frequency Chest Wall Oscillation in Chronic Obstructive Pulmonary Disease Patients with Mucus Hypersecretion,” a study published in International Journal of Chronic Obstructive Pulmonary Disease, applied HFCWO to a group of 22 elderly patients suffering from moderate to severe COPD with excessive mucus secretions. In as little as four weeks, HFCWO was able to improve the patients’ quality of life and reduce disease symptoms.
Researchers have been perfecting the science of matching HFCC settings to patients to optimize care. A study from Children’s Hospital of Pittsburgh of University of Pittsburgh Medical Center, “Resonant Frequency Does Not Predict High-Frequency Chest Compression Settings That Maximize Airflow or Volume,” investigated how HFCC vests could be set to match the intrinsic frequency of patients’ breathing patterns. Research clinicians measured the natural resonant frequency of patients’ chests using impulse oscillometry. They also studied the frequency of HFCC vests during use, as well as the frequency of HFCC vests that produced the greatest volume and flow of air.
After collecting data, the clinicians identified that 32 of the patients studied used HFCC with a median frequency of 14 Hz, and a large majority used 15 Hz or 12 Hz. This did not match the patients’ own resonant frequencies, which were a median of 20.3 Hz. A selected 19 patients underwent the optimization study for maximum volume and flow, and it was found that the median measures were 8 Hz and 26 Hz, respectively. Surprisingly, none of the parameters tested were correlated. No independent variables could predict what frequencies provided patients with maximum volume or air flow, indicating that further optimization and tuning is required to help patients using HFCC.