A new experimental model — the social amoeba known as Dicty — may greatly help researchers understand the mechanism by which cells in airway passages protect themselves against cigarette smoke, and advance needed research into chronic pulmonary diseases tied to smoking.
The model’s discovery, presented by Corrine R. Kliment and colleagues from Johns Hopkins University in Baltimore during ASCB 2015, the annual meeting of the American Society for Cell Biology held earlier this month in San Diego, California, is detailed in a study titled “Cytoskeletal and Mitochondrial Genes as New Targets in the Protection of Airway Epithelial Cells Against Cigarette Smoke.”
Chronic obstructive pulmonary disease (COPD) describes a group of lung diseases — including chronic bronchitis, emphysema, and chronic obstructive airways — that are a major cause of morbidity and mortality worldwide. Air pollution and other airborne irritants can be factors in COPD development, but cigarette smoking is unequivocally its main cause. There is no cure for COPD, and novel treatment targets are urgently needed since standard therapies have limited effect on disease progression or mortality.
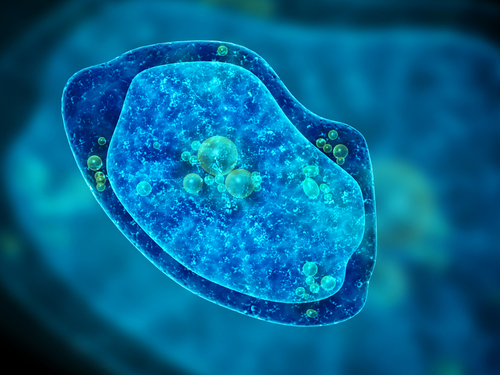
The research team found two new surprising such targets in the amoeba models they chose to study the effects of cigarette smoking. The social amoeba Dictyostelium discoideum, or Dicty, they thought a particularly good model for human COPD, since it reacts robustly and predictably to cigarette smoke or to its laboratory form, cigarette smoke extract (CSE). Dicty, studied alongside human bronchial epithelial cells, opened potential ways to identify new pathways and therapeutic strategies that might protect the airways against cigarette smoke (CS).
The team found that CS, used as an oxidative insult, led to cytoskeleton and metabolism modifications in the amoebas. CS extract (CSE) slowed the growth rate of Dictyostelium discoideum in a concentration‐dependent manner. The researchers were able to identify Dicty genes that seemed to offer a protective effect against CSE. For this, they used a cDNA library to screen over 30,00 transformants that led them to 10 genes, covering three cell pathways — cytoskeleton, metabolism, and genome/translation — that protected against CS‐induced growth defects.
They focused on two genes: Actin‐interacting protein‐1 (Aip1), involved in changes in the cell cytoskeleton, and the ADP/ATP translocase (AncA), which is critical for mitochondrial ATP transport involved in cell metabolism. The AncA gene has well-known paralogs in humans, the ANT genes. By reintroducing the two genes into the amoebas, the researchers restored protection against CSE‐induced growth defects. They also used human bronchial epithelial cells (HBEKTs) to evaluate the impact of 10% or 20% CSE exposure. They observed that both insults induced ANT1 expression, indicating a cellular protective effect by ANT. Moreover, increasing the expression of ANT2 in human HBEKTs led to higher cell viability and preservation of cell morphology after CSE treatment.
Overall, this study combined the benefits of two model systems, human lung epithelium and the amoeba Dictyostelium discoideum, to offer a powerful new approach to discovering the pathways involved in COPD biology as well as strategies that might lead to new COPD therapies.