Targeting a rare population of cells within the lungs may inhibit the hyperactivity of lung immune responses that underlie several diseases, including asthma. The study, “Pulmonary neuroendocrine cells function as airway sensors to control lung immune response,” was published in the journal Science.
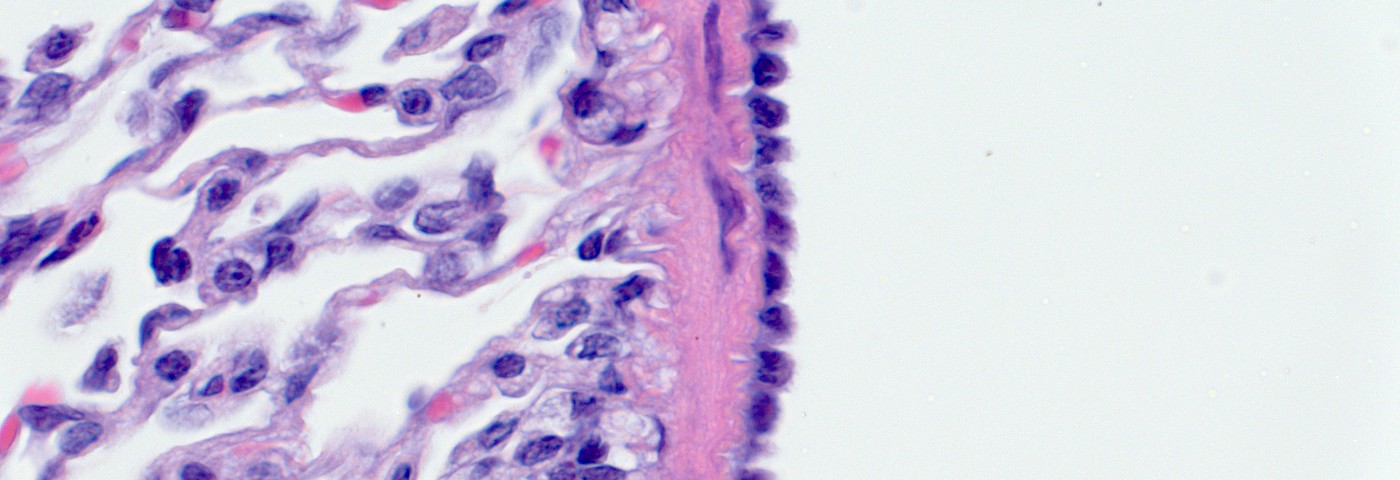
Lungs are constantly exposed to environmental atmospheric cues, but how lungs respond to these cues has been poorly understood. Pulmonary neuroendocrine cells (PNECs) are a rare group of lung epithelial cells previously linked to a wide range of human lung diseases, including asthma, pulmonary hypertension, cystic fibrosis, even sudden infant death syndrome.
Now, a research team at the University of Wisconsin-Madison investigated the function of PNECs function in a living organism and discovered they act as sensors within the airway of many animals, including humans.
“These cells make up less than 1 percent of the cells in the airway epithelium. Our conclusion is that they are capable of receiving, interpreting and responding to environmental stimuli such as allergens or chemicals mixed with the air we breathe,” Xin Sun, UW-Madison medical geneticist and the study’s lead author, said in a press release.
The team focused on the role of a pair of genes known as ROBO1 and ROBO2. Mutations in both genes are implicated in a severe disease known as congenital diaphragmatic hernia (CDH), where newborns have a hole in their diaphragm, the muscle that controls breathing, thereby allowing the organs in the abdomen to reach the chest. Despite the fact that babies can recover after surgical intervention, there is still a significant number of newborns who die. In the babies who survive, some can suffer symptoms similar to asthma or pulmonary hypertension.
Researchers discovered that when they “knock-out” ROBO1 and ROBO2 genes in mice, they could reproduce human congenital diaphragmatic hernia, but also observed that pulmonary neuroendocrine cells became disorganized. In healthy controls, PNECs formed clusters of cells. “In the mutant, they don’t cluster. They stay as solitary cells, and as single cells they are much more sensitive to the environment,” Sun said.
Moreover, PNECs in the mutant mice increased neuropeptide (small protein molecules that are potent regulators of the immune response) production upon exposure to air. Since PNECs are the only known cells in the airway epithelium that are linked to the nervous system, these results showed that they act as sensors, retrieving information within the lungs and sending it to the brain and vice-versa. Neuropeptide overproduction is linked to disorders of the immune system, such as asthma.
The study concludes that strategies regulating PNECs carry a high potential for therapeutic value in lung diseases.