In a new study, researchers at the University of North Carolina discovered that alveolar macrophages — specific immune cells — and a protein called XBP-1 are responsible for the exacerbated inflammation responses observed in cystic fibrosis (CF) patients.
The results offer new therapeutic avenues and favor the theory that inflammation and other specific symptoms are an acquired response instead of direct consequences of mutations in the CFTR gene. The paper, “X-Box-Binding Protein 1 and Innate Immune Responses of Human Cystic Fibrosis Alveolar Macrophages,” was published in the American Journal of Respiratory and Critical Care Medicine.
CF is caused when two defective copies of the CFTR gene are inherited. This chronic, genetic and life-threatening disease affects the respiratory and digestive systems. The CFTR protein normally acts as a chloride channel, transporting chloride ions across cell membranes and contributing to the production of mucus, which protects the lining of the airways.
CFTR mutations result in a defective protein and, consequently, in a deficient chloride ion transport, leaving CF patients more vulnerable to infections by several pathogens.
Respiratory viral infections represent an important cause of morbidity in CF patients, who also experience exacerbated inflammation. Researchers have long debated if the inflammatory state is preceded but not caused by the genetic mutation, or if such symptoms are a direct cause of defective CFTR gene copies.
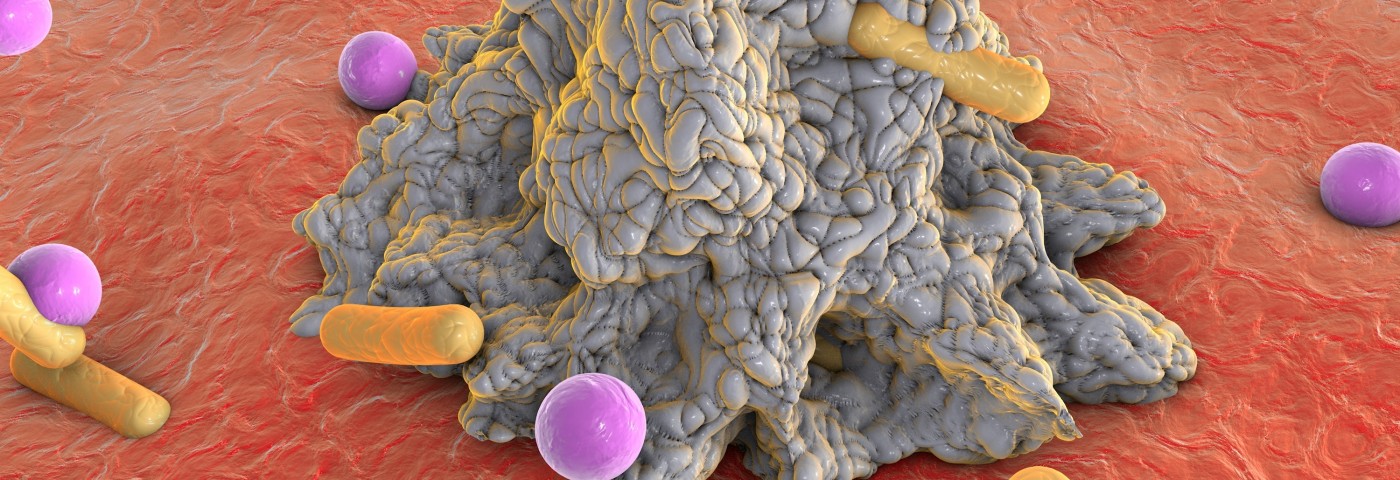
Based on this doubt, scientists have now investigated alveolar macrophages (AMs), immune cells that are essential for the host defense to inhaled bacterial pathogens, and that exert their protective activity through the secretion of inflammatory cytokines.
Moreover, researchers tested if the X-box–binding protein-1 (XBP-1), previously shown to have a key role in inflammation at other sites, is required for inflammation driven by the alveolar macrophages.
The team studied AMs from human cystic fibrosis lungs and healthy lungs. Cystic fibrosis AMs showed an increased basal inflammatory response when compared to the AMs from healthy lungs.
Moreover, when stimulated with cystic fibrosis factors, both sets of immune system cells responded, but the response from cystic fibrosis AMs was greater. The same pattern was observed regarding XBP-1 expression, raised in both sets of cells, but a larger response was observed in cystic fibrosis AMs.
Overexpression of XBP-1 in normal macrophages led to the exacerbated inflammatory profile found in cystic fibrosis macrophages. On the other hand, inhibition of XBP-1 led to the downregulation of the inflammatory response. Importantly, inhibition of CFTR function did not elicit a cystic fibrosis-like response in the macrophages from healthy lungs.
Together, the results led researchers to suggest that the inflammatory response observed in cystic fibrosis is likely acquired instead of a direct consequence of the CFTR mutation.
“Our work has shown that the alveolar macrophage plays a key role in the pathogenesis of cystic fibrosis airway inflammation,” the study’s senior author, Dr. Carla Ribeiro, said in a press release, “and that activation of XBP-1 mediates the secretion of inflammatory factors by alveolar macrophages. This is all helping to make a stronger case for why this pathway may be an important target for therapy.”