In a new study, researchers at Rice University in Houston and the University of Texas MD Anderson Cancer Center demonstrated for the first time that some aggressive lung cancer cells associated with difficult-to-treat diseases have lost immunoproteasome expression, which translates into significantly reduced antigen presentation and results in immune system evasion.
Researchers found that reduced expression of the immunoproteasome is associated with and can predict poor clinical outcome in non-small-cell lung carcinoma (NSCLC) patients. The research article, “Immunoproteasome deficiency is a feature of non-small cell lung cancer with a mesenchymal phenotype and is associated with a poor outcome,” was published in the journal Proceedings of the National Academy of Sciences.
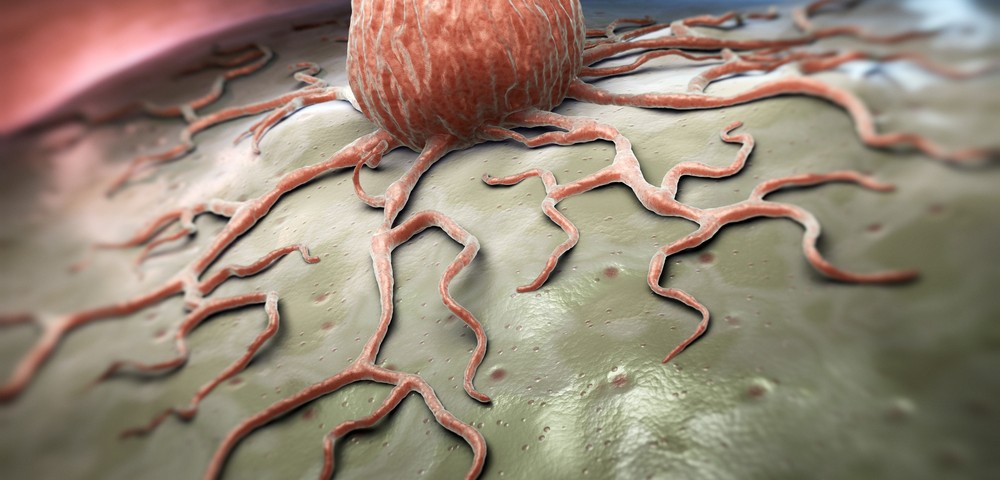
Immunoproteasomes, key signalers of the immune system’s T-cells for recognition and attack of tumor cells, are produced inside cells and degrade unwanted or damaged proteins, such as those produced by invading pathogens. These degraded pieces of protein bind to cell surfaces, forming structures that signal T-cells of the nature of the disease.
Researchers analyzed data gathered over the years and found that patients with early stage non-small-cell lung cancer — the most common type — who have low levels of immunoproteasome expression are more likely to have recurrent and metastatic cancers. Moreover, the team found that this low expression is associated with transition from epithelial-type cells, which bind to each other to form skin and organ linings, to free-floating mesenchymal-type cells, which are known to be more resistant to chemotherapy and immunotherapy treatments.
The research team also profiled protein expression in different cancer cell lines and correlated it to patient outcome, developing computer models that allowed them to rapidly combine and evaluate protein-signaling pathways as the disease progressed.
“The idea was to leave no stone unturned. We modeled the changes in gene expression that can be readily measured, how they might be caused, and how these are correlated to all the other changes going on in the cells,” Dr. Herbert Levine, the study’s co-author, said in a press release. “We want to go from the basic biology of defining the circuits and how they change the expression of these key proteins to showing that they really do have a consequence in terms of recognition by the immune system.”
From all the studies, researchers concluded that immunoproteasome suppression is a consequence of feedback loops activated by the transition to mesenchymal-type cells. Importantly, researchers achieved induction of the immunoproteasome with IFNγ or 5-aza-2′-deoxycytidine (5-aza-dC) treatment — results that may have substantial relevance to the development of effective strategies to target tumor cells with inherent resistance to T-cell-mediated immunotherapy.