The American Sleep Apnea Association (ASAA) announced that the Patient-Centered Outcomes Research Institute (PCORI)’s Board of Governors has approved $2.5 million in funding for a three-year demonstration project titled “Monitoring and Peer Support to Improve Treatment Adherence and Outcomes in Patients with Overlap Chronic Obstructive Pulmonary Disease and Sleep Apnea.“
The American Sleep Apnea Association (ASAA) announced that the Patient-Centered Outcomes Research Institute (PCORI)’s Board of Governors has approved $2.5 million in funding for a three-year demonstration project titled “Monitoring and Peer Support to Improve Treatment Adherence and Outcomes in Patients with Overlap Chronic Obstructive Pulmonary Disease and Sleep Apnea.“
The project will be incorporated with a Large PCORnet Collaboration, and is more simply known as the O2VERLAP Study. The award’s approval is conditional on completion of a business and programatic review by PCORI staff, and issue of a formal award contract once the vetting process is complete.
ASAA, founded in 1990, is a patient-led 501(c) nonprofit dedicated to sleep health promotion through research, advocacy, and education. Most recently, ASAA released its SleepHealth Mobile App Study on Apple’s ResearchKit platform to study sleep health and its connection to general health, safety, and productivity (more on SleepHealth below). PCORI is an independent, nonprofit organization authorized by Congress in 2010 with a mission to fund research that will provide patients, caregivers, and clinicians with evidence-based information needed to make better-informed healthcare decisions.
This multi-partner demonstration project will evaluate the relative effectiveness of proactive care (for example, web-based peer coaching education and support intervention) relative to reactive care in improving patient adherence to nighttime oxygen and positive airway pressure (PAP) therapies in patients who have been diagnosed with both chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea (OSA).
The O2VERLAP Study observes that PAP therapy and oxygen are both effective OSA treatments, but many patients don’t use them as prescribed, or have not been educated regarding good self-management practices. The study is patient-driven by a collaboration of stakeholders motivated to participate in patient-centered research. The aim is to encourage and inform better healthcare decisions that lead to the sort of improved outcomes that matter most to patients while exploring ways to build PCORnet’s infrastructure through exciting studies.
The O2VERLAP’s primary goal is to test the comparative effectiveness of two strategies designed to improve adherence and patient outcomes in patients who use oxygen and PAP therapy: a proactive two-way web-based platform guided by a peer and pro coach, and a reactive referral to the same educational content without the support and two-way interaction.
O2VERLAP will also collaborate with other PCORnet groups and external stakeholders to explore new models for stakeholder engagement, the use of new technologies, crowdsourcing methods, and more. The study will also investigate the comparative effectiveness of the two intervention groups in improving patient-centered outcomes such as sleep quality and symptoms.
The study investigators noted that both COPD and OSA are common chronic disease conditions that affect the lives of millions of Americans, and separately contribute to the morbidity and mortality of hundreds of thousands of people annually. Moreover, they observed that 10-15 percent of COPD patients also have OSA in what is called overlap syndrome — a condition that carries with it more complications. Individuals with overlap syndrome who do not use PAP therapy have an increased risk of death and more hospitalizations from acute exacerbations, emphasizing the importance of treatment.
O2VERLAP results will provide clinicians with guidance in seeking the best strategies for removing barriers to treatment adherence and for promoting efficient educational and patient coaching platforms. The study results are also anticipated to help patients understand the benefits of their treatment, and to effectively provide guidance for using social media, peer-to-peer support, Apple ResearchKit iPhone apps, and viral messaging in the recruitment and enrollment of new study participants, the ultimate objective being the improvement of patient infrastructure for PCORnet and its Commons.
The study abstract notes that collaboration within PCORnet has revealed significant commonalities among many patient communities, especially in COPD and OSA, such as breathing difficulties, anxiety, and depression, and similar challenges faced in creating research infrastructure. O2VERLAP is expected to provide insights that will help in directly addressing challenges being encountered by PCORnet networks: recruitment, retention, co-enrollment, collaboration, and sustainability.
The researchers have assembled a group of partners committed to participating in O2VERLAP to prioritize outcomes, develop study protocols, cross-recruit for the study, and create practical study dissemination strategies, in addition to exploring best practices for cross-network governance structures, enrollment, and data-sharing.
“Other PCORI-funded projects have shown that peer support is successful in increasing PAP adherence and my own research has shown that a group self-management approach led by a sleep provider with sleep apnea facilitating group support sessions results in an increase in PAP adherence,” said Carl Stepnowsky, Ph.D., O2VERLAP co-principal investigator, an associate professor at the University of California at San Diego, and ASAA’s chief science officer, in a press release.
“This line of research has resulted in an approach called the Sleep Apnea Self-Management Program, which will be the basis of the material and content for this intervention,” he said.
The O2VERLAP project will also include engaging patient partners and stakeholders in a program of focus groups and interviews to help them better understand treatment barriers and important outcomes, and help refine development of a peer-led internet-based coaching program to improve adherence and other patient-centered outcomes for people with both COPD and OSA.
The project also reunites ASAA with five patient-powered research networks (PPRN) and one additional clinical data research network (CDRN) that are members of PCORnet, two professional medical associations, and three patient-centered home medical companies.
These partners include:
- The COPD PPRN
- The Health eHeart Alliance PPRN
- The American BRCA Outcomes and Utilization of Testing Patient- Powered Research Network (ABOUT) PPRN
- The Population Research in Identity and Disparities for Equality
- Patient-Powered Research Network (PRIDEnet PPRN)
- PI Patient Research Connection (PI-CONNECT) PPRN
- Patient-Centered Scalable National Network for Comparative Effectiveness Research (pSCANNER) CDRN
- American Thoracic Society
- American College of Chest Physicians
- The VGM Group
- CMB Solutions
- Evermind
“COPD and sleep apnea are two chronic conditions that impact the lives of millions of Americans. These two comorbid conditions are of increasing concern to each of our patient communities and this project was born out of our collaboration with different patient-advocacy groups, especially the COPD Foundation,” said Adam Amdur, ASAA’s chief patient officer and patient co-investigator. “We are extremely honored to be working with our great PCORnet partners and other dear colleagues in this study and we look forward to engaging other new partners through our Sleeptember campaign.”
Sleeptember is a new ASAA yearlong project to connect the dots between quality of sleep and other health conditions through fun and engaging online and community events. Sleeptember’s discussion forum enables patients from various disease communities and other stakeholders to crowdsource research ideas, educational needs, messaging, and promotional and dissemination ideas to gain additional support and funding for research.
In support of this effort, the ASAA and its partners will create online resources to educate patients and other stakeholders about patient-centered research and explain why it’s in their best interest to be involved. These will include videos, graphics, blogs, and testimonials written by patients and others, and offered through several dynamic engagement platforms.
 One such platform is SleepHealth — an iPhone App Study and Wellness tool from the ASAA, powered by Apple’s ResearchKit and IBM Watson Health Cloud. The SleepHealth study is being conducted by the ASAA in collaboration with researchers at the University of California at San Diego, and the app and study were designed and funded through contributions of a small all-patient team of scientists, physicians, advocates and technology experts, all dedicated to health and data discovery as a means of accelerating patient-centered and citizen research related to COPD and OSA, as well as heart disease, hypertension, obesity, cancer, depression, Alzheimer’s, motor-vehicle crashes, and reduced quality of life among others.
One such platform is SleepHealth — an iPhone App Study and Wellness tool from the ASAA, powered by Apple’s ResearchKit and IBM Watson Health Cloud. The SleepHealth study is being conducted by the ASAA in collaboration with researchers at the University of California at San Diego, and the app and study were designed and funded through contributions of a small all-patient team of scientists, physicians, advocates and technology experts, all dedicated to health and data discovery as a means of accelerating patient-centered and citizen research related to COPD and OSA, as well as heart disease, hypertension, obesity, cancer, depression, Alzheimer’s, motor-vehicle crashes, and reduced quality of life among others.
 The SleepHealth app is a personalized tool that helps the user gain greater insight into their sleep habits and sleep issues, to learn how sleep is associated with other conditions, and help take charge of these influences on your health. SleepHealth users can track their daily activities, sleep habits and daytime alertness in order to better understand how sleep impacts their health, safety, productivity, and well-being. The O2VERLAP researchers want anyone who sleeps — restfully or otherwise — to use the SleepHealth app and contribute to the study over a period of years.
The SleepHealth app is a personalized tool that helps the user gain greater insight into their sleep habits and sleep issues, to learn how sleep is associated with other conditions, and help take charge of these influences on your health. SleepHealth users can track their daily activities, sleep habits and daytime alertness in order to better understand how sleep impacts their health, safety, productivity, and well-being. The O2VERLAP researchers want anyone who sleeps — restfully or otherwise — to use the SleepHealth app and contribute to the study over a period of years.
The SleepHealth study is unique in that it enables participants to be equal partners in both monitoring their symptoms and quantifying their impact of sleep loss, as well as helping to direct future research through participating in the community forum at http://www.sleeptember.org, or engaging with the SleepHealth Blog right from their iPhone.
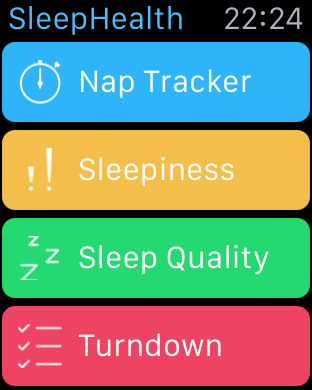 The app can help you measure your activity through the sensors in your iPhone, iPod touch, Apple Watch, or any wearable activity device linked to HealthKit. By helping you track your activity levels and giving you feedback, the project’s aim is to help people become better informed and empowered in ways to improve their health.
The app can help you measure your activity through the sensors in your iPhone, iPod touch, Apple Watch, or any wearable activity device linked to HealthKit. By helping you track your activity levels and giving you feedback, the project’s aim is to help people become better informed and empowered in ways to improve their health.
SleepHealth app Key Features:
Record and track your:
- Physical activity through your iPhone or a HealthKit-linked device;
- Alertness level each day using a scale and easy test for reaction time;
- Sleep habits and daytime alertness through morning and evening checks-ins to monitor how the quality and quantity of your sleep affects your daily alertness, productivity, mood and health.
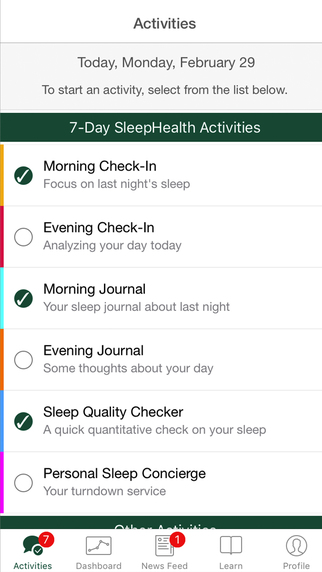 Receive reminders and notifications about:
Receive reminders and notifications about:
- Daily and nightly activities to improve your sleep habits and health;
- Activities and surveys to complete during the 7-Day SleepHealth Activity Check Up every three months.
Get educated:
- Learn about your activity level;
- Learn about sleep health, sleep disorders and their effects on health, safety, and productivity;
- Receive frequent sleep and health tips and news through the SleepHealth Blog right in the app.
To join the SleepHealth Mobile App Study, you must be 18 or older; live in the United States; and be able to read and understand English.
For more information on the SleepHealth Mobile App Study and Sleeptember, visit http://www.Sleeptember.org.
The free SleepHealth Mobile App Study app can be downloaded from the Apple iTunes Store at:
https://itunes.apple.com/us/app/sleephealth/id1059830442?ls=1&mt=8
COPD
COPD refers to a class of progressive, debilitating respiratory conditions that affect an estimated 15 million to 25 million Americans, and more than 300 million people worldwide. It is the third-leading cause of death and the second-leading cause of disability in the United States.
OSA
OSA is a relatively common chronic medical condition characterized by repeated stops or near stops of breathing during sleep. OSA is estimated to affect some 17 percent of U.S. adults and more than 25 percent of older adults, with rates increasing due to the obesity epidemic. Sleep apnea requires immediate therapy because it lowers blood-oxygen levels and is associated with an array of potentially debilitating or fatal disorders such as hypertension, myocardial infarction, stroke, atrial fibrillation, and early mortality. OSA is also associated with increased COPD, depression, anxiety, cognitive issues, erectile dysfunction, irritability, daytime sleepiness, and motor vehicle crashes.