A collaborative study led by Weill Cornell Medicine investigators suggests that starving the immune system might lead to treatments for lung diseases, including chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis (IPF), and asthma. The study, “Arginase 1 is an innate lymphoid-cell-intrinsic metabolic checkpoint controlling type 2 inflammation,“ was published in the journal Nature Immunology.
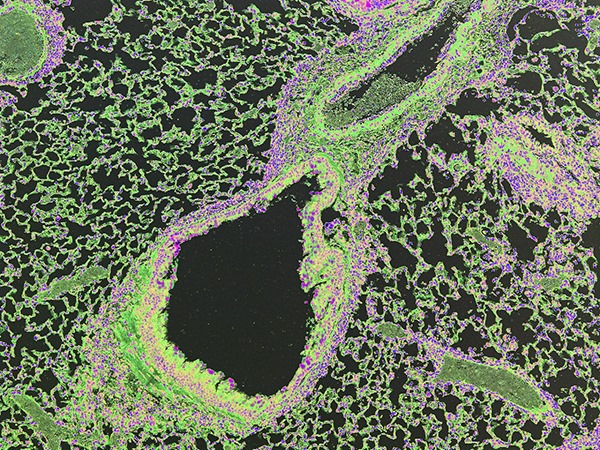
The researchers, led by Dr. Laurel Monticelli, used mice genetically altered to lack Arginase-1 in cells known as innate lymphoid cells (ILCs), which are responsible for allergic reactions. The scientists exposed these mice to an allergen called papain, but the animals did not respond with characteristic lung inflammation or a normal allergic response. The lack of an allergic response was caused by the missing Arginase-1 enzyme. This enzyme is responsible for the breakdown of the amino acid arginine into other metabolic nutrients needed by ILCs; without it, the ILCs were “starved” and unable to function.
“While these are still early days in this research, our patient-based analysis, coupled with our mouse model studies, suggests altering Arginase-1 metabolism within these innate immune cells may offer a therapeutic target for multiple inflammatory diseases,” Monticelli said in a news release.
The investigators also studied human ILCs taken from people with COPD and IPF. They found that these cells in the human inflamed tissues also produced Arginase-1.
“These findings are very exciting and propel us to look deeper into how the immune system is regulated in the context of health and chronic inflammatory diseases,” said senior investigator Dr. David Artis, director of the Jill Roberts Institute for Research in Inflammatory Bowel Disease and the Michael Kors Professor of Immunology at Weill Cornell Medicine.
“This report gives us new mechanistic insight to understand how we might be able to design more selective drugs that specifically target ILCs to treat a range of allergic diseases,” Artis said.
The findings could impact a wide range of diseases in which lung inflammation and allergic reactions occur, including COPD, IPF and allergic diseases, such as eczema, asthma, and life-threatening food allergies.
Allergies cost the U.S. more than $18 billion a year and are the sixth-leading cause of chronic illness in the country. More than 50 million Americans a year suffer from allergies.
The study was supported by several organizations, including the National Institutes of Health (NIH), the Burroughs Wellcome Fund, the Crohn’s and Colitis Foundation of America, the Edmond J. Safra Foundation/Cancer Research Institute, the National Science Foundation, The Robert Wood Johnson Foundation, The Thoracic Surgery Foundation, and the German Research Foundation.
Image: Color-enhanced histologic image of allergen-induced type 2 inflammation in mouse lungs. Photo credit: Dr. Laurel Monticelli and Dr. David Artis.