TGV-inhalonix, Inc., presented data on the drug candidate, Mul-1867, to treat antibiotic-resistant lung infections that is showing promise with the mixed bacterial and fungal infections found in cystic fibrosis (CF) patients. The presentation, from an animal study, was made at the recent 39th European Cystic Fibrosis Conference in Basil, Switzerland.
Mul-1867 is a nebulized solution designed for self-administration. It is the first drug being developed to address mixed bacterial and bacterial-fungal respiratory infections in people with CF.
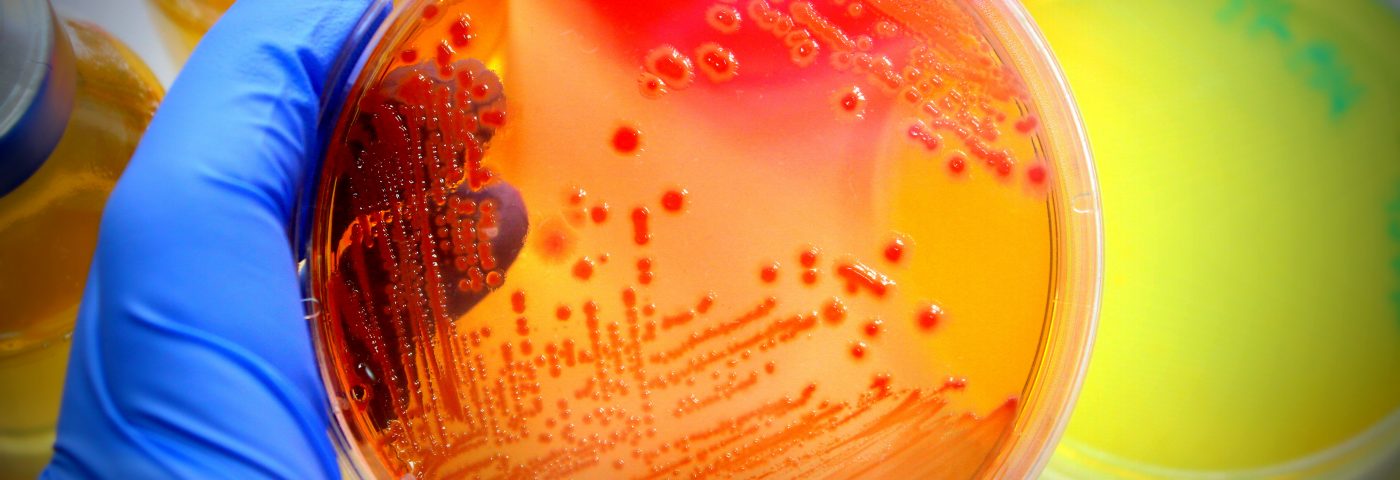
In the study presented, mice with acute and drug-resistant infections — due to bacterial and fungal isolates from CF patients — were treated with inhaled Mul-1867, and the drug was shown to provide 80 percent or greater protection against mortality. The infections came from a mix of Pseudomonas aeruginosa and Staphylococcus aureus bacteria, and P. aeruginosa and the fungi Candida albicans. In comparison, mice treated with an aminoglycoside antibiotic commonly used by CF patients with lung infections had a 50 percent survival rate.
“Mul-1867 is a breakthrough drug candidate that has shown significant promise in treating the chronic infections that lead to progressive decline in lung function and eventually respiratory failure in patients with cystic fibrosis,” Dr. George Tetz, scientific and development advisor for TGV-inhalonix who gave the presentation, said in a press release. “Mul-1867 is the first drug candidate in development that holds promise against resistant strains of bacteria, as well those infections caused by a mix of bacteria and fungi infections that plague cystic fibrosis patients.”
A pilot study of Mul-1867 involving 15 CF patients was recently completed, the company reported on its website.
The U.S. Food and Drug Administration (FDA) has designated Mul-1867 an orphan drug to speed its development and testing.
TGV-inhalonix believes Mul-1867 has the potential to treat respiratory tract infections in chronic obstructive pulmonary disease (COPD) patients, and for ventilator-associated and fungal pneumonia patients.