A new research study titled “Directed vaccination against pneumococcal disease” recently published in the Proceedings of the National Academy of Sciences (PNAS) journal, described a novel vaccine that allows bacteria responsible for pneumonia to colonize in a person’s body, triggering its defensive mechanism only if the bacteria becomes threatening.
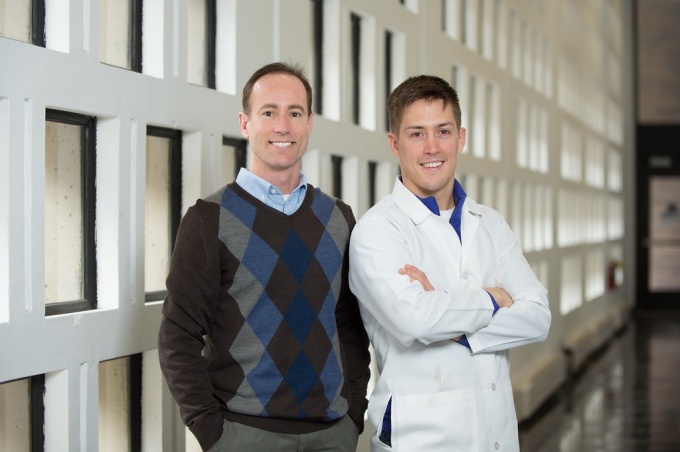
The groundbreaking work of Blaine A. Pfeifer, an associate professor of chemical and biological engineering at the University at Buffalo (UB) School of Engineering and Applied Sciences, and Charles H. Jones, Abcombi Biosciences’ CEO, among others, combines the novel approach with the protein-based vaccine’s potential to neutralize more than 90 strains of the bacteria. This could potentially make the traditional vaccines of Louis Pasteur (the creator of the first vaccine, against rabies) obsolete, since they work by destroying bacteria before colonization.
“With conventional vaccines, the approach has been ‘what bacteria do we want to target and how’” explained Jones in a press release. “Our strategy is to shift the paradigm to which diseases do we want to prevent.”
According to the World Health Organization, pneumonia is the leading cause of death among children worldwide under age age of 5. This new approach offers what could be the most direct and broad response to pneumonia yet discovered. Meningitis, sepsis, and other severe infections caused by Streptococcus pneumoniae (pneumococcus) could also benefit from such a vaccine.
“These are very serious illnesses that we haven’t been able to completely suppress. The vaccine we’re developing could finally get that job done,” Pfeifer said.
The UB and Abcombi vaccine identifies bacterial strains by proteins binding to the surface of pneumococcus. Lab tests have demonstrated that the vaccine can successfully defend a person from more than 12 strains with 100 percent effectiveness at promoting the appropriate immune response. Additional tests are now needed to confirm if the vaccine could potentially be this effective against all strains.
“It’s like the arcade game Whac-A-Mole. Think of the mallet as a traditional vaccine. It can’t stop all the moles, or in our case, all the strains of bacteria at once,” Jones said. “But our vaccine does just that. It’s like a mallet with 90 heads that strikes all the moles simultaneously.”
Jones emphasized that the ability to fight several strains is critical, since the development of new vaccines is always costly and lengthy. The new vaccine allows bacteria to stay in the body as long as it’s not harmful. The approach works by instructing the immune system to attack only if the surfaced proteins release themselves from the bacterial coating.
“That’s the signal that this bacteria is becoming a troublemaker, that it’s threatening the body and that it’s necessary to fight back,” Pfeifer explained.
Clinical studies in animals have proven the vaccine’s effectiveness, and Abcombi is now leading efforts to begin trials in humans.