 A new practical guide has been launched to assist healthcare professionals in the United Kingdom in identifying and managing the nutritional needs of people with chronic obstructive pulmonary disease (COPD) who are at risk of disease-related malnutrition.
A new practical guide has been launched to assist healthcare professionals in the United Kingdom in identifying and managing the nutritional needs of people with chronic obstructive pulmonary disease (COPD) who are at risk of disease-related malnutrition.
The new resource, “Managing Malnutrition in COPD,“ was developed by a panel of professionals with an interest in malnutrition in COPD. It is based on clinical evidence, clinical experience, and accepted best practices, and has been endorsed by 10 key U.K. professional and patient organizations.
The guide includes a pathway for appropriate use of oral nutritional supplements, which are typically used along with a normal diet when the patients’ diets alone are insufficient to meet their daily nutritional requirements.
Authors of the guide say that by using the five-step Malnutrition Universal Screening Tool (MUST), it has been estimated that approximately 21 percent of people with COPD (up to 630,000 people in the U.K.) are at risk of malnutrition, which may develop gradually over several years or more rapidly following exacerbations. Researchers also noted that effectively managing those at risk of malnutrition according to the guidance in the National Institute of Health and Care Excellence (NICE) Quality Standards can result in significant cost savings for the National Health Service of more than £119,000 per 100,000 of the general population in the U.K.
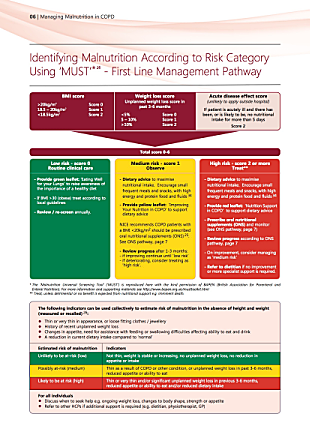 The guide is presented to patients in three complementary color coded patient leaflets (green: low risk, yellow: medium risk, and red: high risk) containing advice on eating choices and physical activity, as well as tips to help cope with common COPD symptoms, such as dry mouth, taste perception changes, and shortness of breath. Additionally the red (high risk) leaflet includes advice for patients on how to incorporate nutritional supplements in their diets.
The guide is presented to patients in three complementary color coded patient leaflets (green: low risk, yellow: medium risk, and red: high risk) containing advice on eating choices and physical activity, as well as tips to help cope with common COPD symptoms, such as dry mouth, taste perception changes, and shortness of breath. Additionally the red (high risk) leaflet includes advice for patients on how to incorporate nutritional supplements in their diets.
 “ARNS has been delighted to be involved in the development of these guidelines and is pleased that we have engaged with the multiprofessional team to ensure that we are offering continuity of nutritional care for patients,” said Matthew Hodson MBE, chair of the U.K. Association of Respiratory Nurse Specialists, one of the organizations involved in the development of the guide, in a press release.
“ARNS has been delighted to be involved in the development of these guidelines and is pleased that we have engaged with the multiprofessional team to ensure that we are offering continuity of nutritional care for patients,” said Matthew Hodson MBE, chair of the U.K. Association of Respiratory Nurse Specialists, one of the organizations involved in the development of the guide, in a press release.
“It is estimated that 1 in 5 patients with COPD will be at risk of malnutrition and identifying and managing it are key to better outcomes and quality of life for patients,” Hodson said. “I think that nurses and other healthcare professionals involved in the treatment of patients with COPD will find the management pathway and the pathway for using oral nutritional supplements invaluable in assisting them in identifying and managing this treatable condition.”
“Patients with COPD who experience weight loss and are of a low body weight will have a poorer prognosis and an increased risk of mortality. Malnourished patients have an increased risk of acute exacerbations, hospital readmission and poor quality of life,” said consultant dietitian Dr. Elizabeth Weekes, NIHR clinical lecturer and the British Dietetic Association’s Parenteral and Enteral Nutrition Group (PENG) representative on the “Managing Malnutrition in COPD” expert panel.
“It is common for stable COPD patients to consume close to the recommended daily amounts for both energy and protein while at home, however, their nutritional intake is often compromised during acute exacerbations,” Weekes said.
“Dietary advice to optimize oral intake is vital for these patients and for those with a low BMI [body mass index], NICE recommends that the diet is supplemented with oral nutritional supplements. This guidance helps healthcare professionals to identify individuals at risk of malnutrition and assists them in implementing an appropriate nutritional care plan. The pathway emphasizes the importance of regular monitoring by healthcare professionals once a care plan is in place to ensure patients meet their nutritional goals,” she added.
PDF copies of the guidance and supporting materials can be downloaded here.

