Researchers at the Perelman School of Medicine at the University of Pennsylvania found that toxins from a type of mold, called aflatoxins, weaken the airways’ self-clearing mechanisms and immunity, which may lead to respiratory diseases and the exacerbation of existing ones.
The findings were reported in a study titled “Fungal Aflatoxins Reduce Respiratory Mucosal Ciliary Function,” published in the journal Nature Scientific Reports.
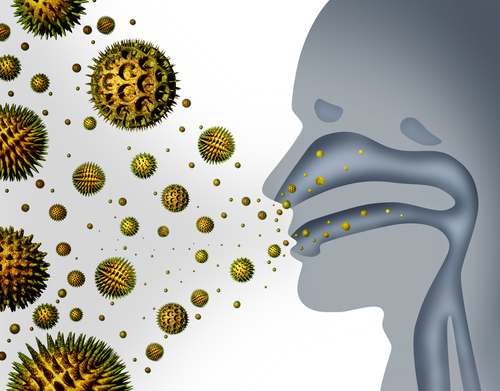
Aflatoxins are mycotoxins produced by fungi, commonly known as molds (Aspergillus, for instance), which are pathogens that can opportunistically colonize the human respiratory tract causing allergic fungal rhinosinusitis and bronchopulmonary aspergillosis. Aflatoxins can be found in certain foods, but humans are usually exposed from contaminated dust that is inhaled during food processing.
In the study, researchers examined the effects of acute exposure to aflatoxins on airway cell physiology, using human upper airway cells (sinonasal and bronchial cells).
The team found that acute exposure to aflatoxins decelerated and weakened key defense mechanisms in the airways, specifically the mucosal ciliary clearance (MCC) and ciliary beat frequency (CBF). Cilia refers to the hair-like structures that line the airways, and which are responsible for cleaning out dust, particles, and microbes.
MCC is the primary physical defense of the respiratory tract against inhaled pathogens. When the MCC fails, respiratory infections can occur and significantly impair the patient’s quality of life.
According to the researchers, the findings indicate that aflatoxins boost fungi development and other co-infecting pathogens, such as bacteria.
“With these defenses impaired, it may create a window of opportunity for the infection, and potentially a domino effect,” lead author Robert J. Lee, PhD, an assistant professor in the departments of otorhinolaryngology – head and neck surgery, and physiology at Penn, said in a news release.
Dr. Noam A. Cohen, MD, PhD, an associate professor of otorhinolaryngology at Penn, said some patients “may become more susceptible to upper respiratory infections and chronic rhinosinusitis (CRS) that can ‘seed’ lower respiratory infections, especially in those with a compromised immune system. It can also exacerbate the more severe lung diseases, such as cystic fibrosis or chronic obstructive pulmonary disease.”
In immunocompromised individuals (chemotherapy patients, for example) or those with damaged airways (such as cystic fibrosis patients), Aspergillus fungi infections can invade the mucosa.
Acute or chronic invasive fungal rhinosinusitis or pulmonary aspergillosis requires aggressive antifungal and/or surgical intervention to prevent mortality. So it is important to study the interaction of Aspergillus with the airway epithelium to better understand the development of fungal respiratory infections. This knowledge is also important for the development of new treatments.
Researchers also found that aflotoxins activate the protein kinase C (PKC). PKC is involved in decreasing ciliary beat frequency, and consequently decrease MCC. According to the team, PKC represents a treatment target.
In their experiments, researchers tested the effects of two PKC inhibitors (Gö6983 and calphostin C), and found that the drugs blocked the reduction in ciliary beat frequency. As a result, PKC inhibitors may be used as a treatment for fungal infections and also to prevent other co-infections.
“PKC inhibitors may decrease fungal respiratory disease and ultimately help alleviate some of those consequences,” Cohen said.
Additional studies of aflatoxin exposure levels are critically needed to help understand the consequences of both acute and chronic aflatoxin respiratory exposure in both humans and animal models, the researchers said.
“Longer-term studies of the effects of aflatoxins will help to shed light on situations of chronic exposure and effects on airways,” the team concluded.

Thank you for bringing to light a growing problem due to both interior and exterior environmental issues.
I am so impressed by this study. I test homes for a living and find high or elevated counts of these toxins in over 85 % of homes. This is an area of medicine where the surface has not been scratched. Now how to disseminate this medical information to the hands of those treating? What is the process? When my clients head to the pulmonologist, they have little understanding of the many neurological affects as well as long term affects of living on a water damaged building. Get antifungals is next to an impossible feat. Thank you for this research. May you further study these toxins. Tricothecenes as well. Thank you! Thank you!