 In an abstract presented during American Thoracic Society 2014 International Conference, entitled “Pulmonary Functional Imaging Of Bronchiectasis: A First Look At Ventilation Abnormalities And Their Relationship With Pulmonary Function And Symptoms,” S. Svenningsen and colleagues from the Robarts Research Institute at The University of Western Ontario in Canada presented their clinical evaluation in subjects with a clinical diagnosis of bronchiectasis using 3He MRI ventilation distribution for the first time.
In an abstract presented during American Thoracic Society 2014 International Conference, entitled “Pulmonary Functional Imaging Of Bronchiectasis: A First Look At Ventilation Abnormalities And Their Relationship With Pulmonary Function And Symptoms,” S. Svenningsen and colleagues from the Robarts Research Institute at The University of Western Ontario in Canada presented their clinical evaluation in subjects with a clinical diagnosis of bronchiectasis using 3He MRI ventilation distribution for the first time.
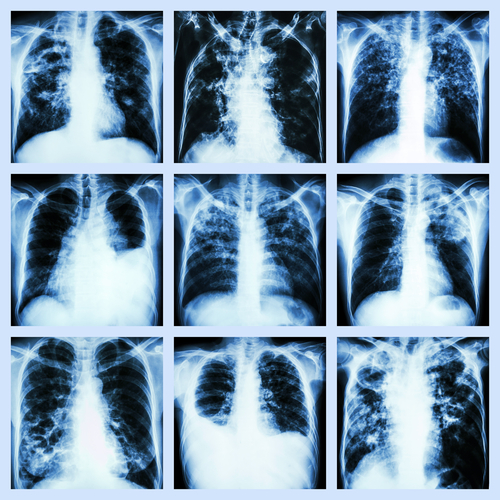
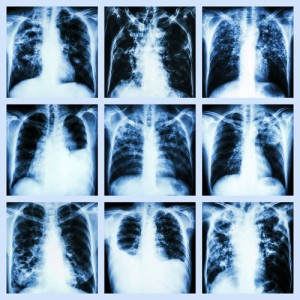
According to the American Lung Foundation, Bronchiectasis is an abnormal stretching and enlarging of the lungs’ airways caused by mucus blockage. The blockage and accompanying infection causes inflammation, leading to the weakening and widening of the passages. The disease can develop at any age, usually beginning during childhood, but symptoms may not appear until much later. It can be congenital or can develop after birth as a result of injury or other diseases, like tuberculosis, pneumonia, and influenza. Some underlying conditions that damage the airways and increase lung infections can cause bronchiectasis such as cystic fibrosis and primary ciliary dyskinesia.
[adrotate group=”6″]
Bronchiectasis cannot be cured. However, with proper treatment, most people can live a normal life. Symptoms include coughing, shortness of breath, abnormal chest sounds, daily production of large amounts of coughed up mucus, chest pain, and clubbing. Early detection is crucial in order to prevent the progression of lung damage. Prevention methods include: vaccinations for measles and pertussis; avoiding toxic fumes, gases, smoke and other substances that can harm the lungs; properly treating lung infections in children; avoiding inhaling small objects, and seeking prompt medical care if any of these occur.
Hyperpolarized gas magnetic resonance imaging (MRI) provides an in-vivo assessment of regional gas distribution in the lung and has the advantage of showing exactly where regional functional abnormalities occur. Previous studies in asthma, chronic obstructive pulmonary disease, and cystic fibrosis have revealed heterogeneously distributed lung function abnormalities that are associated with pulmonary function and symptoms, however, 3He gas distribution has not been evaluated in non-CF bronchiectasis.
In order to evaluate 3He MRI ventilation distribution, subjects with a clinical diagnosis of bronchiectasis were used to test the hypothesized that MRI pulmonary function abnormalities are related to pulmonary function and symptom scores. The team of researchers evaluated 14 (aged 45-85 years) patients using spirometry, plethysmography, the six-minute walk test (6MWT), hyper polarized 3He MRI, high-resolution computed tomography (HRCT), Patient Evaluation Questionnaire (PEQ), and the St. George’s Respiratory Questionnaire (SGRQ).
Using linear regression and Pearson correlations the most novel finding from this study is that MRI heterogeneously distributed ventilation abnormalities are strongly related to worse pulmonary function and symptom scores. This is a pioneering study as this was the first time this method is used in this particular clinical population. The new findings can help physicians to have a better understanding of the key characteristics of Bronchiectasis in diagnosis and treatment.