 On December 23, 2014, scientists from the University of Texas Health Science Center at San Antonio published a new study describing a novel way that a bacterial toxin might contribute to asthma and other pulmonary diseases, both chronic and acute. This new understanding could lead to treatments for these medical problems. The research appeared in mBio, an online journal published by the American Society for Microbiology.
On December 23, 2014, scientists from the University of Texas Health Science Center at San Antonio published a new study describing a novel way that a bacterial toxin might contribute to asthma and other pulmonary diseases, both chronic and acute. This new understanding could lead to treatments for these medical problems. The research appeared in mBio, an online journal published by the American Society for Microbiology.
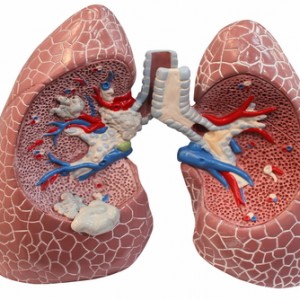
The bacteria, Mycoplasma pneumoniae, is called M pneumoniae, for short. It is a common infectious agent found in the lungs and airways, and produces a toxin known as Mycoplasma pneumonia Community Acquired Respiratory Distress Syndrome (CARDS) toxin. The toxin was discovered at the University of Texas Health Science Center at San Antonio in 2006, and is the first bacterial respiratory toxin identified since diphtheria and pertussis.
The CARDS toxin is produced in the airways, where it interacts with NALP3. NALP3 regulates inflammation and a type of cell death that is genetically programmed and determined; known as apoptosis. Together, these molecules cause an assortment of medical problems.
But if NALP3 is so problematic, why does it exist in the body at all?
[adrotate group=”3″]
According to one of the study authors, Joel B. Baseman, Ph.D., professor of microbiology and immunology in the School of Medicine at the UT Health Science Center and director of the Center for Airway Inflammation Research (cAIR), “Inflammation is important for self-protection from infection and any injury, but when a microbial factor such as the CARDS toxin controls inflammation, bad things happen. Through this mechanism, CARDS toxin triggers exaggerated and prolonged inflammation that results in tissue injury, airway narrowing, mucus hypersecretion, wheezing and coughing.”
Santanu Bose, Ph.D., study co-author and associate professor at Washington State University added, “Because M. pneumonia infections occur so frequently in children and adults and CARDS toxin is such a powerful inducer of inflammation, it is likely that co-infections involving M. pneumoniae, CARDS toxin and other respiratory pathogens result in enhanced severity of disease.”
“Now that we have identified this pathway of disease development, our goal is to prevent the wide range of airway pathologies caused by CARDS toxin with drugs, vaccines and protective antibodies,” said an additional study co-author Thirumalai R. Kannan, Ph.D., associate professor/research in the Department of Microbiology and Immunology at the UT Health Science Center and a cAIR member. “We are undertaking those studies now.”
In 2011, The National Institute of Allergy and Infectious Diseases granted $11.5 million to fund this work, led by Dr. Baseman. It is additionally funded by The Robert J. Kleberg, Jr. and Helen C. Kleberg Foundation.
The discovery sheds new light on how several respiratory diseases may develop. Prevention and treatment strategies based on this work, and that target CARDS toxin, may soon follow.

