Researchers at the Spanish National Cancer Centre and Complutense University of Madrid in Spain recently revealed that telomeres, structures that protect chromosomes, are associated with the genesis of idiopathic pulmonary fibrosis. The study, entitled “Mice with Pulmonary Fibrosis Driven by Telomere Dysfunction,” was published this July in Cell Reports. This study showed for the first time that telomere damage seems to be a cause of disease.
Idiopathic Pulmonary Fibrosis (IPF) is a disease of the lung characterized by a progressive scarring of the lung tissue that leads to a decrease of functional lung volume and oxygen uptake. The origin of IPF is not known, although it can be attributed to a combination of genetic and environmental hazards, like radiation, smoking or pollution, which highly increases the risk of developing the disease. Many people live only 3 to 5 years after diagnosis and the disease currently has no cure. The main cause of death of IPF is respiratory failure. The acute exacerbation of IPF (AE-IPF) has an extremely poor prognosis and is believed to occur per year in 5-10% of patients with IPF.
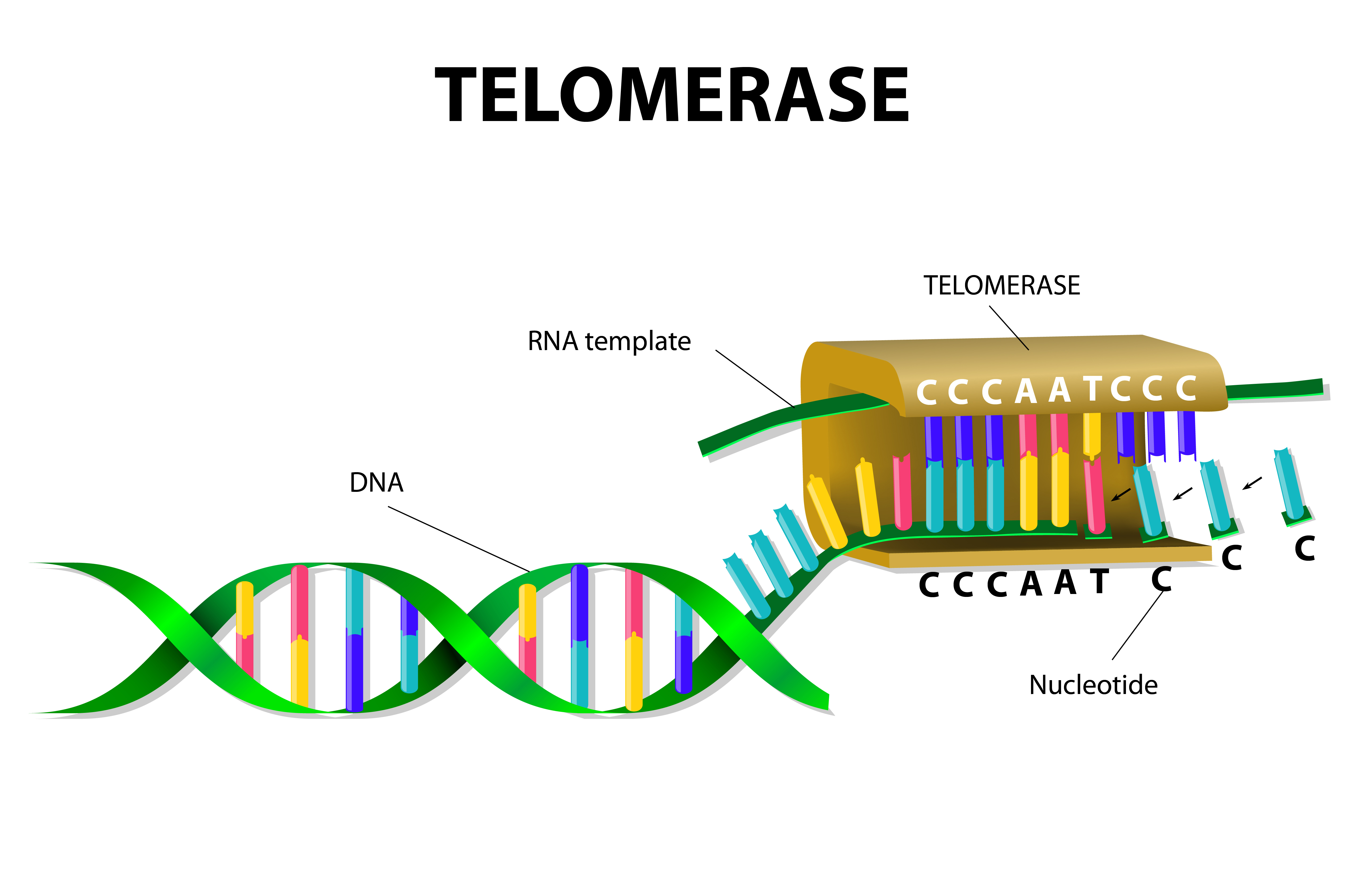
Telomeres, which are protective structures at the ends of chromosomes, have for long time been associated with aging. One important piece of evidence of aging in mice and humans is the progressive shortening of telomeres with increasing age. Previous observations, such as telomeres from patients with idiopathic pulmonary fibrosis being shorter than normal, have already suggested the involvement of telomeres in idiopathic pulmonary fibrosis. Additionally, pulmonary fibrosis is a condition commonly associated with individuals who have mutations in genes implicated in telomere preservation. These findings suggest a strong link between telomere defects and IPF, but the cause-effect connection was not fully understood.
To prove the cause-effect relationship between telomeres and the development of IFP, the research team generated a mouse model that did not have a protein essential for the generation of telomeres in type II alveolar cells, which are crucial for lung tissue regeneration. They observed that the majority of these mice had progressive pulmonary fibrosis.
Paula Martinez, a co-author of the study, said in the news release that severe telomere damage is sufficient to induce pulmonary fibrosis even without using environmental triggers of damage.
The mouse model without telomeres in pulmonary epithelial cells proved the importance of telomeres in the origin of fibrosis, but did not reproduce the disease in most human patients. Therefore, the team generated an animal model that combined early shortening of the telomeres due to telomerase deficiency with low doses of environmental damage. They used bleomycin to induce telomere damage. This drug affects the DNA of cells and blocks cell division when given in high doses. The authors used low doses that were not sufficient to cause pulmonary fibrosis in normal mice.
They found that neither the shortening of the telomeres alone nor low doses of bleomycin alone were enough to cause IPF, but both factors combined were able to cause the disease.
“These findings support a model in which persistent damage derived from short or dysfunctional telomeres is added to other cellular damage and this triggers pulmonary fibrosis,” said Juan Povedano, first author of the study.
The authors concluded that understanding the molecular mechanisms that lead to the shortening of telomeres, a common process seen in aging, enabled the generation of new mouse models that will pave the way for the development of therapeutic strategies based on the activation of telomerase, the enzyme that repairs telomeres, to treat a disease for which there is still no therapy.