Researchers at Columbia University have found a way to bioengineer a “working” lung — a very complex structure — with a viable and intact blood vessel network that can support studies of lung cell repair and stem cell transplants, aiding both research into lung diseases and, potentially, the availability of donor lungs.
The team, led by Gordana Vunjak-Novakovic, director of the Laboratory for Stem Cells and Tissue Engineering, recently published it findings in the journal Science Advances in a study titled “Functional vascularized lung grafts for lung bioengineering.”
“We developed a radically new approach to bioengineering of the lung,” Vunjak-Novakovic, who is also a professor of medical sciences at Columbia, said in a news release.
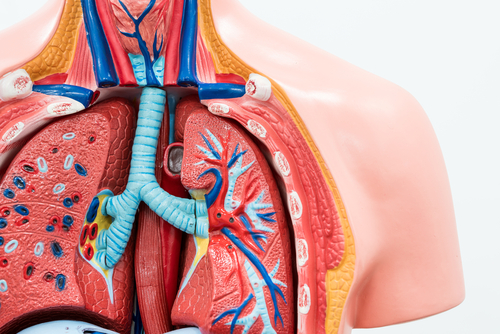
With more than 40 different cell types and a large airway and vasculature surface area, the lung is an incredibly complex organ. It has been a challenge to find ways to promote lung repair to treat advanced lung diseases, the third leading cause of death worldwide.
In contrast to previous bioengineering projects that required an extensive reconstruction of the lung’s vasculature, the team showed it is possible to recreate the pulmonary epithelium while preserving its main structural elements, including such supporting such as fibroblasts, myocytes, chondrocytes, and pericytes. The epithelium is tissue that lines the cavities and surfaces of organs and blood vessels.
“We reasoned that an ideal lung scaffold would need to have perfusable and healthy vasculature, and so we developed a method that maintains fully functional lung vasculature while we remove defective epithelial lining of the airways and replace it with healthy therapeutic cells,” Vunjak-Novakovic said. “This ability to selectively treat the pulmonary epithelium is important, as most lung conditions are diseases of the epithelium.”
The research team used an ex vivo lung perfusion system (EVLP) in a rodent, and delivered to the lung a mild detergent solution to remove lung tissue-specific cells while protecting the remaining structures and other types of cells.
EVLP works in ways similar to the extracorporeal membrane oxygenation (ECMO) system used to support patients in cardiovascular and respiratory failure. EMCO bypasses the lungs to provide the body with necessary oxygen and promote gas exchange in an externally controlled system.
Using its system, the team created a lung scaffold with functional bronchial and vascular architecture. These structures were able to support the attachment and growth of human adult and stem cell-derived pulmonary cells.
Researchers think the bioengineered lung model can help with lung repair, and also help to improve the number of transplantable lungs by making donor lungs more resilient and durable, said Matthew Bacchetta, at associate professor of surgery at the Columbia University Medical Center, and a study co-author.
The team is now testing its approach to study lung development and repair in disease, and to develop new targeted therapeutics. They are also focused on developing new imaging-guided lung evaluation strategies for clinical applications.
This research project was supported by a $8.2 million, seven-year grant from the National Institutes of Health that aims to support research into the mechanisms and treatment of idiopathic pulmonary fibrosis, a serious lung disease.
“This is a major step forward in bioengineering lungs,” Vunjak-Novakovic said. “The creation of de-epithelialized whole lungs with functional vasculature may open new frontiers in lung bioengineering and regenerative medicine.”

This would be awesome
This would be great